Intake progress notes are part of the documentation in hospitals, clinics, and assisted care facilities. This type of document records any changes or instances that happen to the patient and how these affect their situation. The information in the notes is used by physicians or nurses to update any medical care administered to the patient. Read the article to know more about how to write intake progress notes.
3+ Intake Progress Note Samples
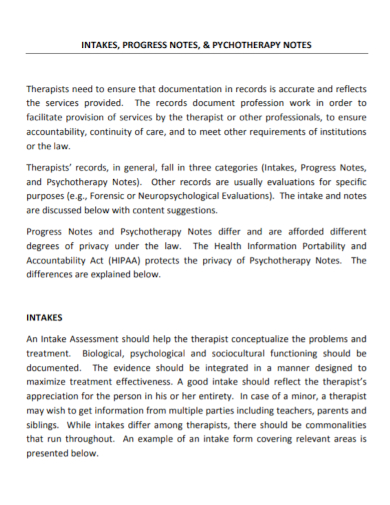
1. Psychotherapy Intake Progress Note
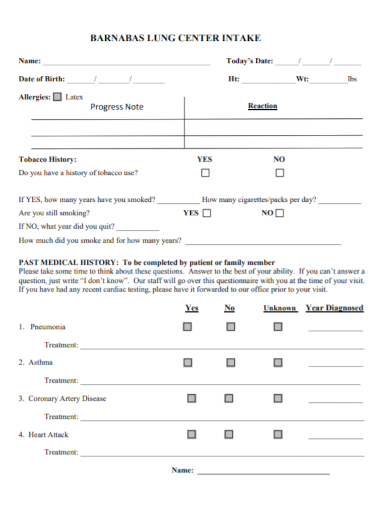
2. Lung Center Intake Progress Note
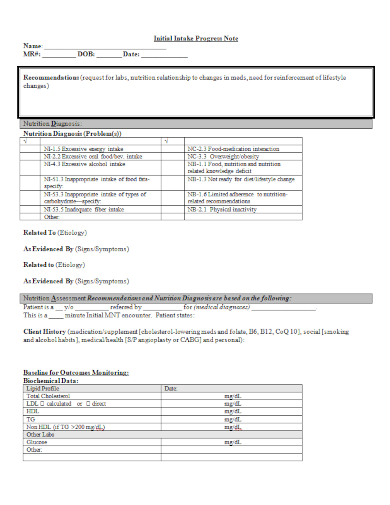
3. Nutrition Initial Intake Progress Note
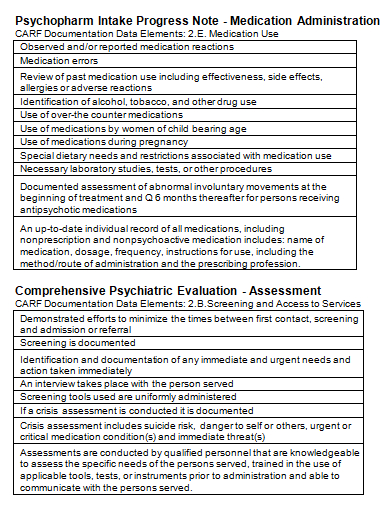
4. Psychopharm Medication Intake Progress Note
What is an Intake Progress Note?
Intake progress notes basically enumerate all the patient’s urgent medical needs at the time of intake note-taking. It could also be taken by physicians, therapists, and lifestyle coordinators to observe patient’s health, behavior, physical appearances, and changes in movement, and abilities during their interaction.
How to Make Intake Progress Note
Intake Progress Notes must always be:
- Concise: Your notes must consist of only one page. Use few and relevant words to convey the information.
- Objective: Only write straight facts based on the information given and your observations. Avoid being subjective in your notes. Jot down anything that you heard or seen, who caused and initiated the situation.
- Relevant: Don’t beat around the bush. Get to the point right away.
To write your intake progress note, make use of your critical thinking skills to assess and analyze the situation. Make sure to see everyone’s point of view of the situation. Your note-taking could be based on answering these important questions:
- What happened?
- Who is involved in the situation?
- What was the reason/cause of the situation? Is there any motive for the situation to happen?
- Who witnessed the situation? How did it happen according to their observation?
Take note that these types of questions are likely to be answered in a subjective manner. Listen well and be objective in taking down the information. Formulating your conclusion from facts. These questions will likely be answered in a subjective manner. Listen attentively and then use your reasoning to be objective and draw conclusions based on facts. Provide recommendations if needed.
Writing Tips for Progress Notes
Intake progress notes should be read at the start of each shift of any staff, so they should have a clear understanding of what kind of support the patient will require.
Your progress notes must be well written. Write legibly and clearly. Make sure you use the correct spelling of words and names. Use the correct sentence structure and make sure your grammar is free from errors. Try to avoid making abbreviations, jargon, and acronyms. Use active voice when writing down your notes. Use a third-person point of view for your notes. When writing down any assistance the staff did for the patient, start the sentence as if writing a procedure.
Make sure to write everything that happened in the session. Write it down as soon as possible. If you fail to write down an instance in the notes, it just basically means that it didn’t happen at all. If the progress note of a client is continuous, make sure to refer to previous entries for continuity. This is important for anyone to read to understand the notes. Make sure the notes written are accurate. If you make a mistake, just cross it out.
FAQs
What is an intake in counseling?
An intake in clinical psychology counseling occurs when a client will seek help first from the physician. The physician will probe questions to the client to know what bothers him and get his symptoms.
How long is an intake session?
An intake session can average between 90-110 minutes. An intake session is more thorough compared to other clinical sessions.
What is the purpose of an intake form?
The purpose of the intake form is to obtain accurate and timely information from a new patient in order to diagnose the patient correctly.
Always remember that a progress note has confidential information about the client. It should not be read just by anyone except the staff who are authorized to do so. Keep the notes in a secure location. If the note is on a computer, make sure the authorized staff has the access to it. If you need some sample format to follow, download our sample intake progress notes templates above. They are free, so you can download any templates you like.
Related Posts
FREE 27+ Daily Log Samples
FREE 17+ Sample Doctors Note
FREE 12+ Sample Mileage Log Forms
FREE 12+ Sample Diet Plan
FREE 11+ Doctor's Note for Work Samples
FREE 9+ Sample Parent Teacher Conference Forms
FREE 6+ Massage Therapist Resume samples
FREE 6+ Sample Weekly Exercise Plan
FREE 5+ Printable Doctor's Note for Work Samples
FREE 49+ Claim Forms
FREE 45+ Medical Forms
FREE 44+ Assessment Forms
FREE 39+ Log Templates
FREE 25+ Sample Daily Reports
Project Evaluation Objectives