Do you need to effectively record the progress of the patient’s therapy or treatment plan? As a medical professional or physical therapist, you need to conveniently write down the progress of the patient’s recovery state. By using this method, it will save you many hours of time-consuming paperwork. Also, it will ease the communication among other healthcare providers. If you are currently learning your way in the medical field , this article will be helpful for you in writing the progress note or SOAP note of your patients. So, we include some blank SOAP note templates to guide you in your healthcare work. Keep on reading!
FREE 10+ Blank Soap Note Samples
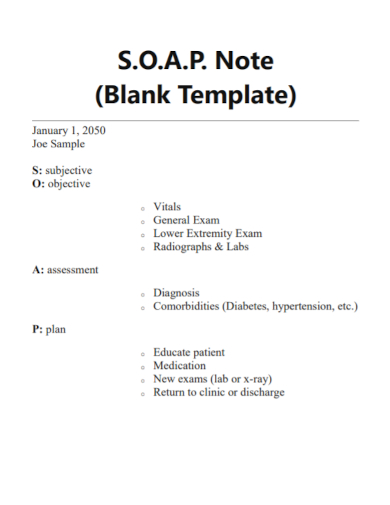
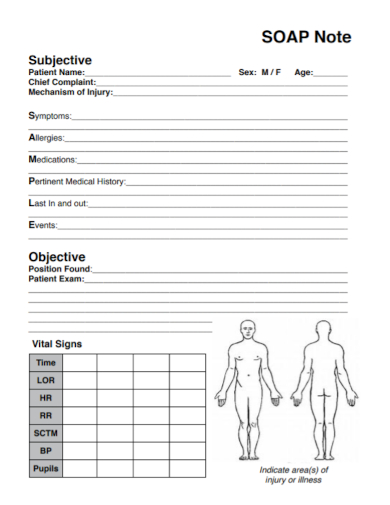
1. Blank Soap Note
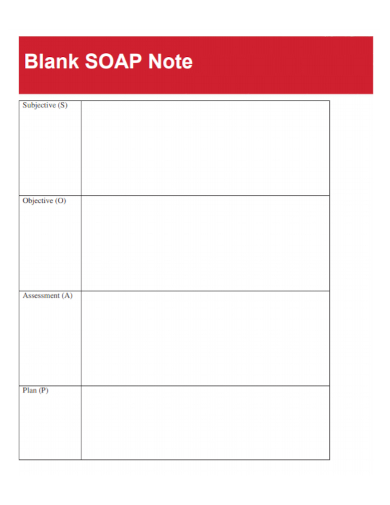
2. Blank Documentation Soap Note
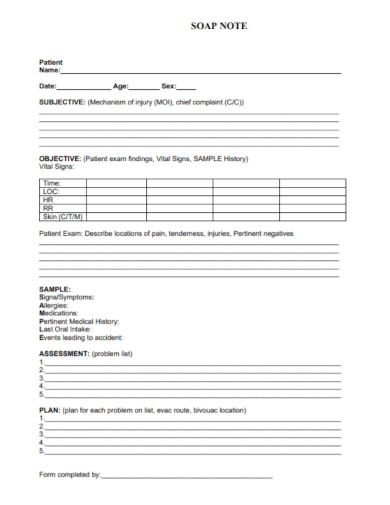
3. Patient Blank Soap Note
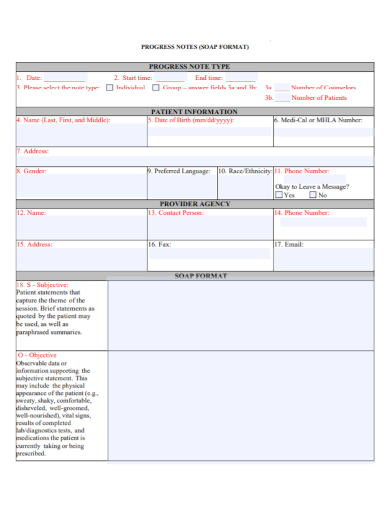
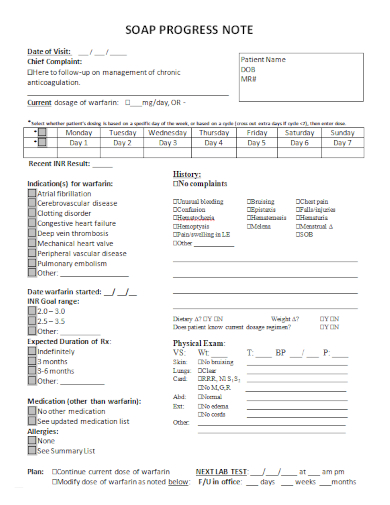
4. Blank Soap Progress Note
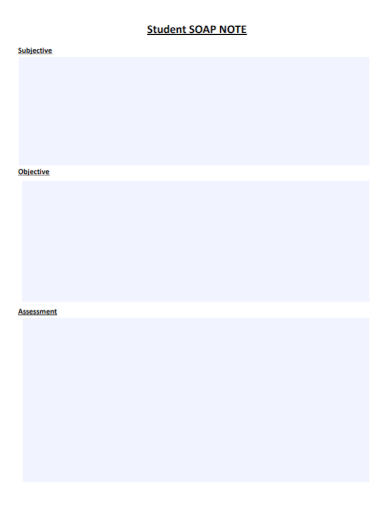
5. Student Blank Soap Note
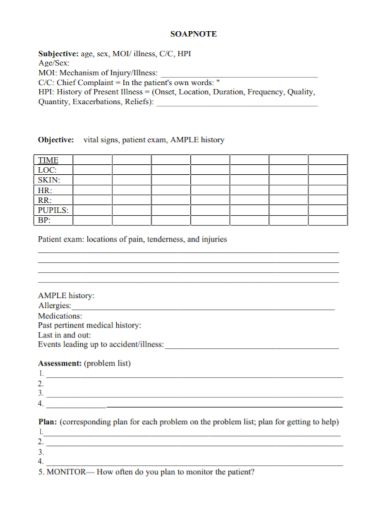
6. Blank Assessment Soap Note
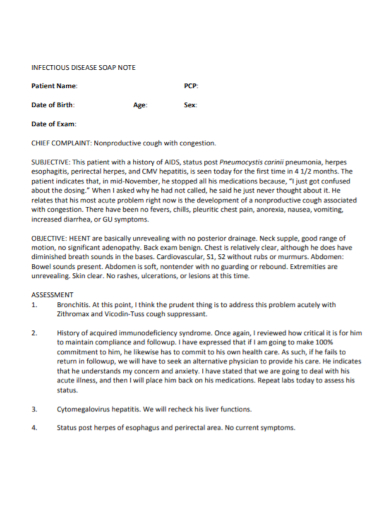
7. Infectious Disease Blank Soap Note
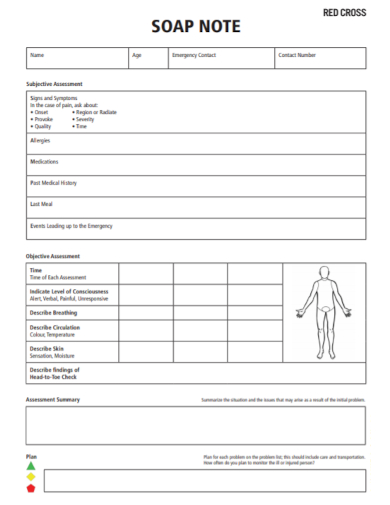
8. First Aid Blank Soap Note
9. Practitioner Blank Soap Note
10. Medical Care Blank Soap Note
11. Blank Patient Soap Progress Note
What is a SOAP Note?
Also known as a DAP (Data, Assessment and Plan) and client progress note, a SOAP (Subjective, Objective, Assessment and Plan) note demonstrates a short and comprehensible medical overview of each therapy or treatment session of the patient and a well-detailed record of the effects of the therapy or treatment plan to the patient.
Moreover, it is an important document that presents solid goals and objectives, as well as the whole development or entire progression of your patient’s physical therapy, rehabilitation for mental health due to drug and alcohol abuse, accidents, trauma, or any other causes.
How to Write a SOAP Note
While you are doing your best effort on facilitating several types of treatments for your patients, you also need to be able to write a clear and in-depth progress report or SOAP note of your clients to examine and closely monitor their individual progress and show feedback to the clients and their guardians or parents about the progress in their therapy or treatment plan.
In this section, we give you some easy-to-follow tips that indicate how to design a comprehensive SOAP note for your patients:
1. Have a good and friendly relationship with the patient
By using some helpful questions to ascertain and bring out your patient’s real thoughts, and feelings, you can understand the condition of your patient. Most importantly, you need to think about having a good relationship with your client to promote change and more progress. Constantly review your methods.
Keep on doing your best effort when you show warmth and friendliness to your client. Make eye contact and allow time for small talk. Then, ask your client about his or her problem.
2. Create assessment of your patient’s needs
After starting the discussion with your patient, you can now create some assessment of your patient’s needs. Research about the diagnosis you made based on his or her physical, emotional, and mental condition.
Take note of the methods and prescriptions that are crucial for your patient’s therapy or treatment plan. Include all of this information to the SOAP note as this will be the starting phase of his or her progress of the medical treatment.
3. Clarify the results of the therapy
Then, after several weeks of the therapy, clarify the results of the therapy in detail. Take note of the new symptoms that he or she is currently feeling due to the intake of some medications. Use some charts, graphs, tables and other visual diagrams while you make some medical interpretations of the patient’s condition after taking the treatment.
Conduct some careful observations of your patient for another week or even months, depending on his or her medical condition. Record every little bit of your patient’s progress in your note. Ask the patient’s parents or guardians about his or her condition at home, at school, etc.
4. Use some psychological evaluation tests
Psychological evaluation tests or assessments are fundamental tests that you need to conduct so that you are able to measure the progress of your patient. This series of tests is a beneficial tool in collecting information about how your clients think, feel, behave, and react. The findings are used as references to develop a medical report or a progress note of your patient’s abilities and behaviors, and creating recommendations for his or her treatment.
FAQs
When writing an effective SOAP note, you need to search for the right time in recording the progress of the client’s treatment session, keep using a professional tone, don’t use complex or complicated terms and phrases, avoid the use of negative phrasing, maintain your notes clear and brief, avoid confusing pronouns, and continue writing with accuracy without judgment.How to write a SOAP note?
A SOAP note contains the subjective, objective, assessment, and plan. It documents the chart of a patient along with the admission note. What is the format of a SOAP note?
The recorded notes are significant to the therapists because they can get back or review the essential details and noteworthy aspects of the therapy process, as they remember the recent accomplishments that were made by the patient and monitor the progress of the therapy.Why do therapists record notes?
A client’s psychological health records which include the SOAP notes must be kept by all licensed psychologists or mental health therapists for a minimum of seven years from the discharge date of the patient or seven years after a minor patient becomes 18 years old. How long do I need to keep SOAP notes?
Therefore, writing a SOAP note for your client is a crucial method in promoting productivity and sustaining order in your job as a nurse, doctor, physical therapist or health professional. Being widely used by a variety of medical and rehabilitation professionals, SOAP notes clearly demonstrate improvement in the client’s functioning and provides structure to medical record entries. Additionally, these notes present logical decision-making with the use of subjective and objective information while determining an assessment and plan for the patient. Here are some of our downloadable and printable blank SOAP note samples available in different kinds of formats.
Related Posts
FREE 5+ Sample Therapy Note
FREE 33+ Doctor Note Samples
FREE 11+ Absence Note Samples
FREE 9+ Medical Note Samples
FREE 9+ Sample Daily Note
FREE 9+ Sample Progress Note
FREE 8+ SOAP Note Samples
FREE 8+ Sample Cornell Note
FREE 8+ Sample KWL Chart
FREE 20+ Sample Cornell Note
FREE 15+ Sample Doctor's Note
FREE 15+ SOAP Note
FREE 8+ Consignment Note Samples
How to Make a Doctor's Note for Work
FREE 5+ Sample Credit Note