In medical terms, DAP stands for Diagnostic Assessment Program. In health-care institutions, this follows the standard organizational format for data, assessment, response, and plan for a patient’s medical care. In a DAP note, clinical notes in the format includes patient contact information, summary, and evaluation of the problem and treatment plan.
Our website offers DAP and doctors note samples that guide users on the proper way of writing DAP notes for patient care plan. These are all free to download, modify, and print for user specifications.
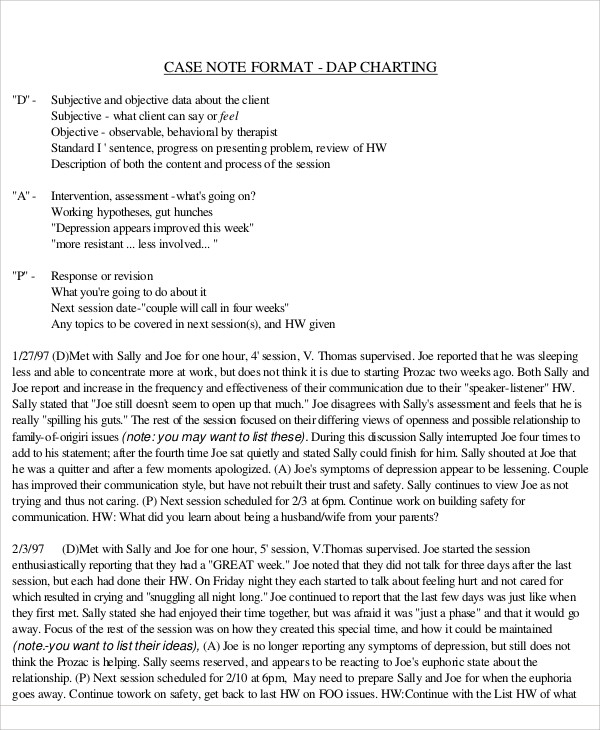
DAP Notes Format
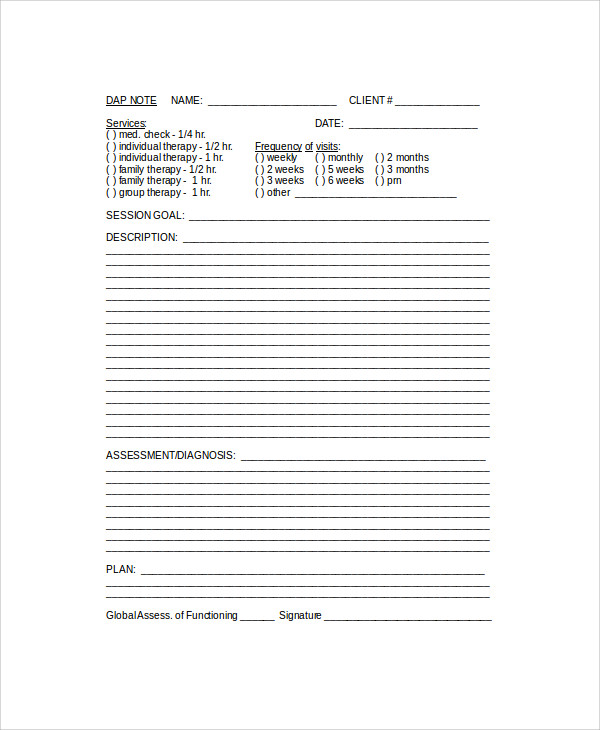
Blank DAP Note
DAP Notes Example
he basic goal of DAP is to make sure all the necessary information, both subjective and objective, are being undertaken for the patient’s immediate care. This includes an assessment based on the the patient’s condition balanced from both subjective and objective analysis. DAP is actually a summary of the more comprehensive SOAP procedure—which stands for subjective, objective, assessment, plan procedure, which is a standard style of documentation used by medical professionals.You may also see Subjective Objective Assessment Planning Notes
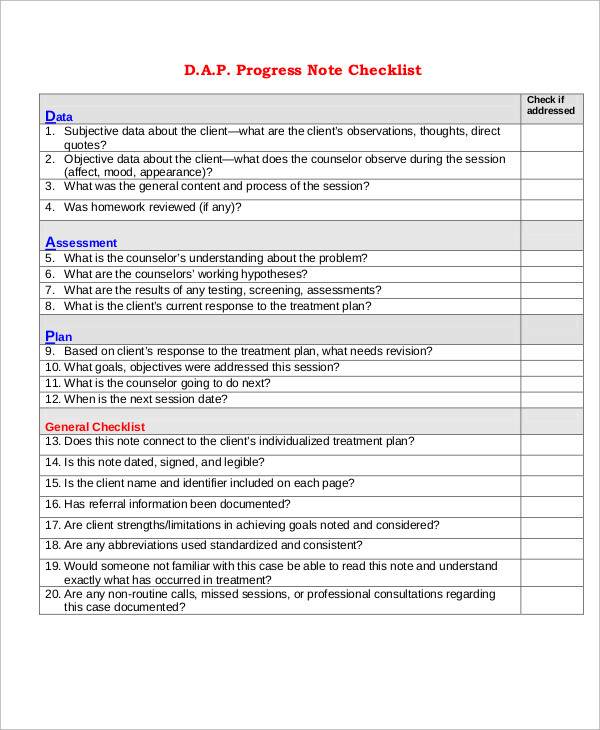
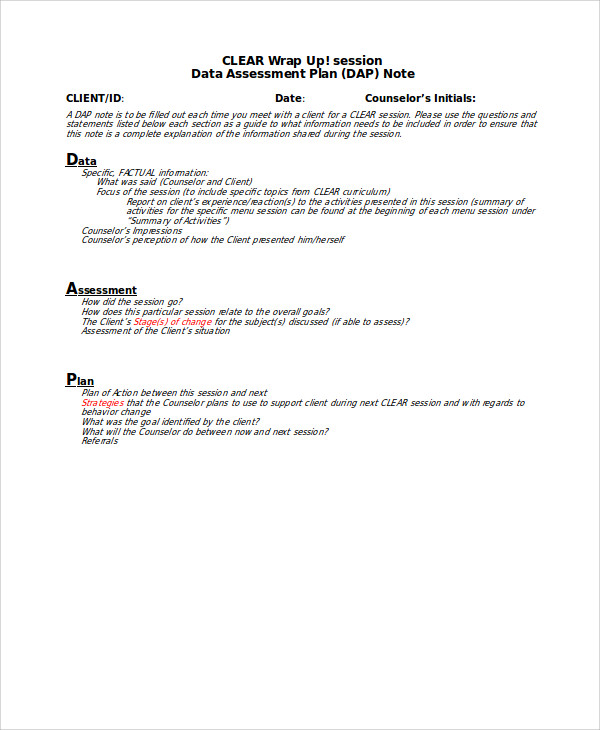
In order to write a standard DAP note, the following procedures must be observed:
Data
1. Subjective Observation
Subjective data on the client based on hat he feels about his ailment, his observations, and thoughts about his condition. The aim here is determine the nature of his pain according to patient’s own description.You may also see delivery note templates
2. Objective Observation
Objective observation based on the health-care provider’s observation on the patient’s condition. Helps to narrow down, isolate, and list the most probable ailment. All observable visual data must be written down including vision, palpitation, circulation, and neurological assessment. This also includes mood and appearance observations.You may also see consignment notes
DAP Progress Notes
DAP Patient Notes Sample
3. Assessment
Recording the Assessment
What the health-care provider’s understanding of the problem and working hypothesis. The likely diagnosis is written on this part in the temporary absence of conclusive diagnosis. Includes results of all screening and testing such as X-rays, blood tests, and possible referral to a specialist. The ailment or injury type should also be recorded whether it’s chronic, acute, or recurring.You may also see thank-you notes for meeting
4. Plan
Write the Plan
Write the necessary steps to treat the patient. The type of treatment given should include medication, therapy, or even surgery. Short- and long-term treatment of the patient should be set as well as change to the lifestyle if necessary. Reducing pain and healing the ailment should be the ultimate goal in the plan. Depending on patient response to the treatment plan, any revisions should also be considered including the number of sessions and the next session date.You may also see thank you notes
For more on medical notes, please refer to more examples on our website or click on the link for Progress Notes Samples. These are all free to download and modify in both Word Doc and PDF files.
Dap Notes in PDF
DAP Notes in Doc
Besides data, assessment, and plan, the health-care provider should make sure to check all the necessary details like patient’s name and identifier and if the note is legible enough for other health-care professionals to understand. Make sure the note is also signed and dated, otherwise the note is not valid. If the patient is being referred to another specialist, make sure this is duly noted and all the necessary information is being documented. Since DAP notes are fully standardized, it’s essential that abbreviations follow the standardized content, otherwise other health-care providers will have a hard time understanding the abbreviations.You may also see sticky notes.
For more detailed assessment notes, please check on our website’s SOAP Notes that can be used for standard forms on making medical assessment and planning.
Related Posts
FREE 14+ Money Promissory Note Samples in PDF
FREE 10+ Thank You Notes For Coworkers Samples in PDF
FREE 10+ Meeting Notes Samples in PDF
FREE 9+ Inpatient Progress Note Samples [ Psychiatric, Hospital, Complaint ]
FREE 10+ Note Taking Samples in PDF
FREE 10+ Credit and Debit Note Samples in PDF | MS Word
FREE 3+ Comprehensive Soap Note Samples in PDF
FREE 8+ Student SOAP Note Samples [ Medical, Pharmacy, Doctor ]
FREE 10+ Return Delivery Note Samples [ Product, Service, Electronic ]
FREE 3+ Car Sale Delivery Note Samples [ Transfer, Private, Vehicle ]
FREE 6+ Goods Delivery Note Samples [ Vehicle, Movement, Return ]
FREE 10+ Doctors Excuse Note Samples [ Office, Visit, Medical ]
FREE 5+ Discharge Summary Nursing Note Samples [ Progress, Patient, Home ]
FREE 6+ Labor and Delivery Note Samples [ Nurse, Progress, Admission ]
FREE 8+ Company Delivery Note Samples in PDF | DOC