According to a study published in the Journal of Patient Safety, ineffective communication is one of “the most common attributable causes of sentinel events.” Given these dire consequences, all clinicians in training should strive to master the ability to convey medical information accurately, clearly, and succinctly. Doctors share medical information in modern clinical practice primarily through oral presentations and written progress notes, which include histories, physicals, and SOAP notes. SOAP notes, which stand for subjective, objective, assessment, and plan, allow clinicians to keep track of ongoing patient encounters systematically.
3+ Comprehensive Soap Note Samples
A comprehensive SOAP note is a type of assessment tool that nurses and others in the healthcare field use. This assessment note contains the specific information required to assess and plan a patient’s medical journey. This type of SOAP note is more specific than a standard SOAP note because it includes a longer narrative of the assessment. It also takes into account all subjective and objective information that is required to make the assessment. Finally, it is a useful tool for learning about a patient’s medical history. This is because it provides all of the necessary information in the order in which it should be completed. Starting with subjective data and working your way to objective data.
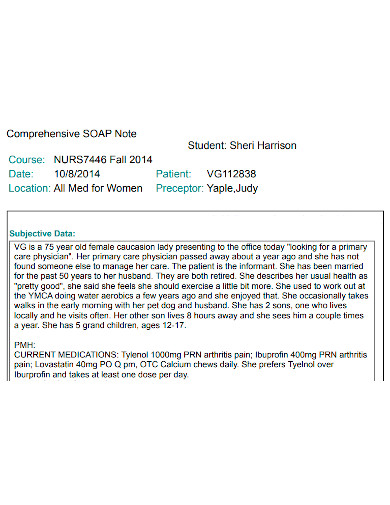
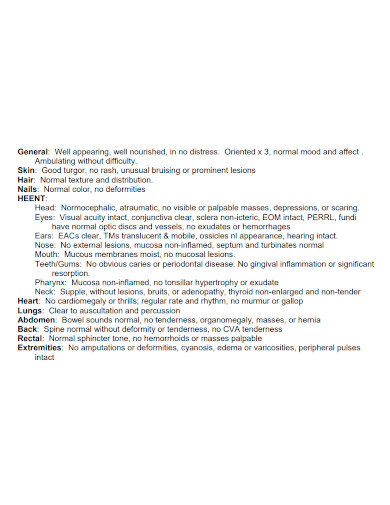
1. Comprehensive Soap Note Sample
2. Printable Comprehensive Soap Note
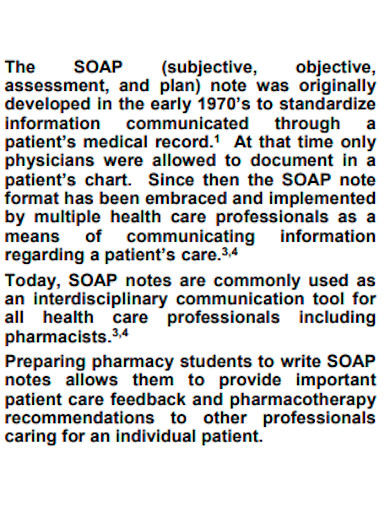
3. Standard Comprehensive Soap Note
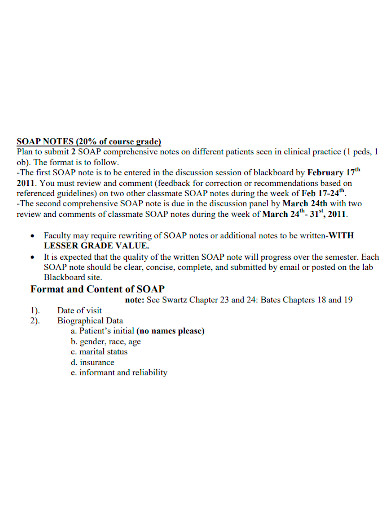
4. General Comprehensive Soap Note
A SOAP note is also a way for nurses, physicians, and anyone else working in the field to save time when learning about a patient’s medical history. It’s also a more convenient way to take notes while doing rounds. It’s also a convenient way for students or medical practitioners to observe, assess, and take notes on medical issues without stopping to write. A soap note can also be beneficial because it allows practitioners to complete an assessment without having to stop and inquire about the patient’s problems. It’s also a good way to come up with a solution without wasting valuable time. When using this method, however, there are a few things to consider. Finally, a comprehensive note is a concise and to-the-point assessment that summarizes the information provided by patients as a means of comprehending their medical history.
Subjective
Start your SOAP note by recording the data you get directly from your patient; don’t add your assessments or interpretations. Include the following in your list:
1. The main complaint of the patient. In their own words, this is what brought the patient to the hospital or clinic.
2. The patient’s current illness history, as reported by the patient. Include details using the acronym OPQRST:
- When the patient’s symptoms first appeared.
- Any factors that are calming or provoking.
- The degree to which the patient’s symptoms are of good quality.
- The affected body region, as well as whether or not there is any radiation (if the pain is a symptom).
- The severity of the patient’s symptoms, as well as any other symptoms that may be present.
- The occurrence of symptoms over time.
3. Important medical information, such as the patient’s:
- Medical and surgical history from the past.
- History of the family.
- History of the social order.
4. A current list of the patient’s medications, including dosages and administration schedules.
Objective
Unsurprisingly, the objective section of your SOAP note should contain objective information gathered during the patient encounter.
1. Begin by taking the patient’s vital signs. Record the temperature, heart rate, blood pressure, respiratory rate, and oxygen saturation of the patient.
2. Now it’s time for your physical examination. Begin with a general impression of the patient, then go over the results of your head, ears, eyes, nose, and throat, respiratory, cardiac, abdominal, and extremity exams, as well as your neurological exam. Include the results of any other relevant exams you’ve taken as well.
3. Any other diagnostics that have been executed should be reported, such as:
- Basic metabolic panels, complete blood counts, and liver function tests are among the laboratory tests available.
- X-rays, computed tomography scans, and ultrasounds are all examples of imaging.
- Any other pertinent diagnostic data, such as electrocardiograms.
Assessment
Report your assessment after you’ve completed the subjective and objective sections of your note.
1. Make a one- to two-sentence summary of the patient’s age, medical history, major diagnosis, and clinical stability. If the patient has multiple major diagnoses, your summary statement should include all of them.
2. Include a differential diagnosis if your patient is experiencing any new symptoms. At least two or three possible diagnoses should be included.
Plan
Fill in the blanks on your SOAP note with your plan.
1. Make a list of all the medical issues that the patient has. Your problem list should be arranged in ascending order of acuity.
2. Make a plan to address each issue you’ve identified. If you’re currently treating a bacterial infection, for example, state that you intend to continue taking antibiotics.
3. If you’re caring for an inpatient, keep track of their deep vein thrombosis prophylaxis, code status, and disposition as well.
FAQs
What does SOAP stands for?
SOAP is an acronym for Subjective, Objective, Assessment, Plan.
What are some of the things that you should avoid when writing a SOAP note?
When you’re in the middle of a session with a patient or client, don’t write SOAP notes. You should keep personal notes for yourself to use as a guide when writing SOAP notes.
What is the importance of medical documentation?
Medical documentation now serves a variety of purposes, and medical notes have grown in length and breadth in comparison to fifty years ago. To meet these demands, medical notes have evolved into electronic documentation. However, one unintended result of electronic documentation is the ease with which large amounts of data can be easily incorporated. If the data isn’t useful, these data-filled notes may become a burden for a busy clinician.
Furthermore, if the information is incorrect, the patient may suffer harm. Making the most clinically relevant information in the medical record easier to find and more readily available is critical. The benefit of a SOAP note is that it organizes this information in a way that makes it easy to find.
Related Posts
FREE 14+ Money Promissory Note Samples in PDF
FREE 10+ Thank You Notes For Coworkers Samples in PDF
FREE 10+ Meeting Notes Samples in PDF
FREE 9+ Inpatient Progress Note Samples [ Psychiatric, Hospital, Complaint ]
FREE 10+ Note Taking Samples in PDF
FREE 10+ Credit and Debit Note Samples in PDF | MS Word
FREE 8+ Student SOAP Note Samples [ Medical, Pharmacy, Doctor ]
FREE 10+ Return Delivery Note Samples [ Product, Service, Electronic ]
FREE 3+ Car Sale Delivery Note Samples [ Transfer, Private, Vehicle ]
FREE 6+ Goods Delivery Note Samples [ Vehicle, Movement, Return ]
FREE 10+ Doctors Excuse Note Samples [ Office, Visit, Medical ]
FREE 5+ Discharge Summary Nursing Note Samples [ Progress, Patient, Home ]
FREE 6+ Labor and Delivery Note Samples [ Nurse, Progress, Admission ]
FREE 8+ Company Delivery Note Samples in PDF | DOC
FREE 5+ Material Delivery Note Samples in PDF