Sample SOAP notes are known as a documentation method used by the health care representative like doctors and nurses for creating a chart about health details of patients. The word SOAP stands for four parts of Nurses and Doctors Note Sample – Subjective, Objective, Assessment, and Plan. The below mentioned SOAP note examples possess the best format for preparing details about the patient’s health in a systematic order. The formats are also editable completely allowing you to enter details you missed out anytime.
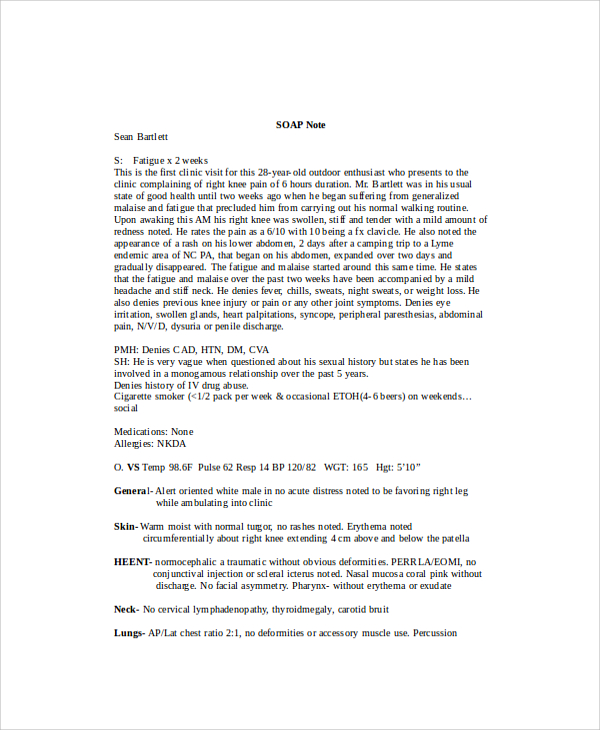
Physical Therapy SOAP Note Example
These SOAP notes are used by the physical therapists or psychotherapists for recording vital information regarding their patient and the proposed treatment measure.
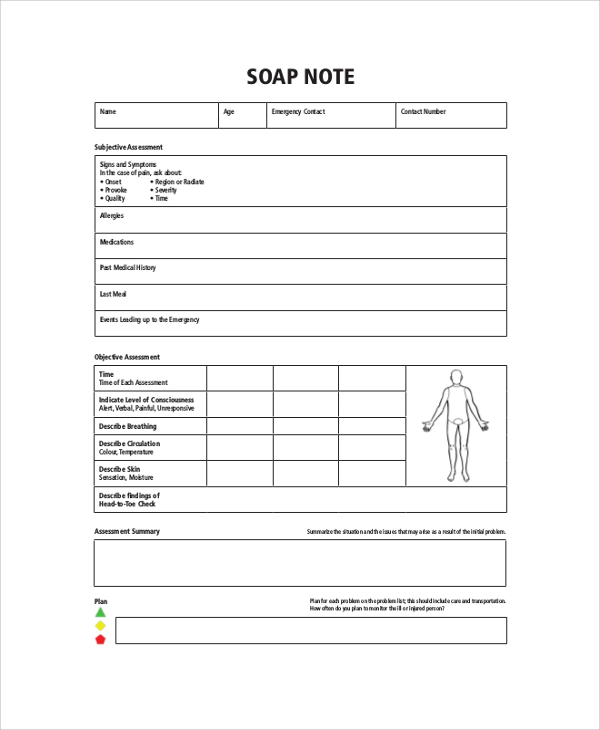
Sample Nursing SOAP Note Example
As the name suggests, this SOAP note is used by nurses. They first examine the patient and jots down all the problems identified in this type of SOAP note. These notes come with a simple preface.
How to Write a SOAP Note?
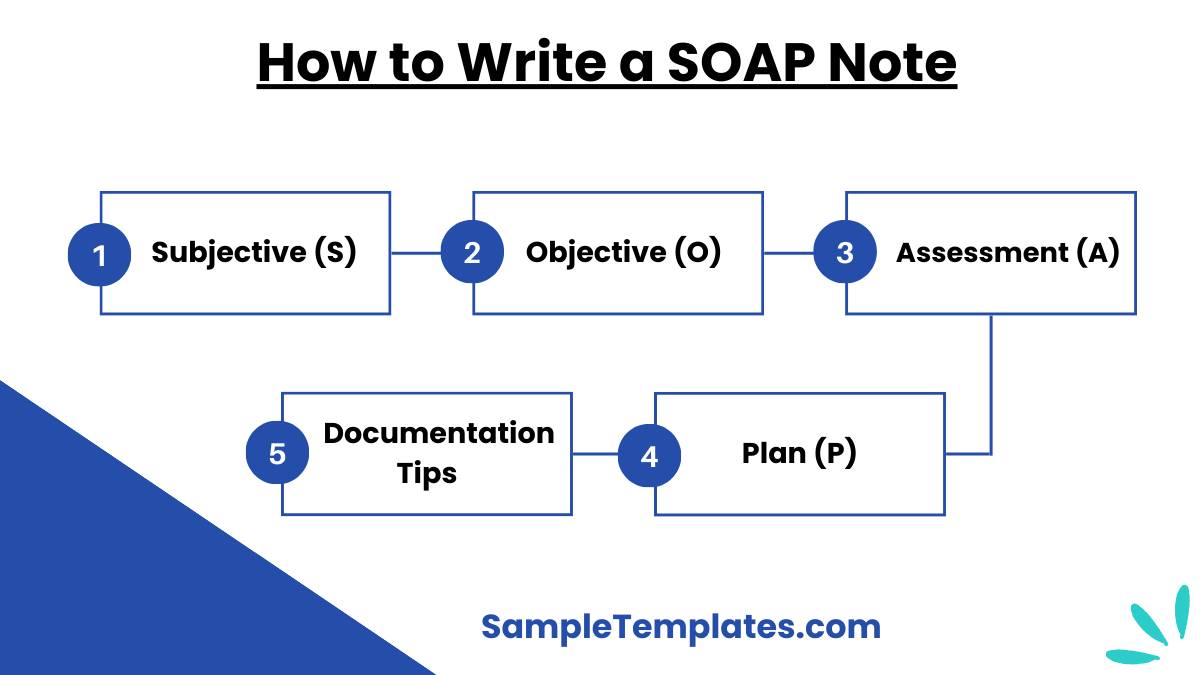
Writing a SOAP note involves documenting patient information in a structured format. SOAP stands for Subjective, Objective, Assessment, and Plan. Here are five points to guide you:
- Subjective (S):
- Record the patient’s chief complaint, history of present illness, and relevant medical history.
- Include any symptoms reported by the patient, such as pain, discomfort, or changes in condition.
- Note the patient’s perspective, including their feelings, concerns, and personal observations.
- Objective (O):
- Document measurable and observable data collected during the physical examination.
- Include vital signs (temperature, blood pressure, heart rate, respiratory rate).
- Record findings from laboratory tests, imaging studies, and other diagnostic procedures.
- Note any physical exam findings, such as appearance, auscultation, palpation, and percussion results.
- Assessment (A):
- Provide a diagnosis or list of potential diagnoses (differential diagnoses) based on the subjective and objective data.
- Summarize the clinical impressions and reasoning behind the diagnosis.
- Mention any progress or changes in the patient’s condition since the last visit.
- Plan (P):
- Outline the treatment plan, including medications, therapies, procedures, and patient education.
- Include follow-up instructions, referrals to specialists, and any additional tests or investigations needed.
- Provide a timeline for the next steps and goals for the patient’s care.
- Address any patient concerns or questions about the treatment plan.
- Documentation Tips:
- Keep the notes concise, clear, and organized.
- Use medical terminology accurately and appropriately.
- Ensure that the notes are legible (if handwritten) and that all entries are dated and signed.
- Maintain patient confidentiality and follow all legal and ethical guidelines for medical documentation. You can also see more on Clinical SOAP Note.
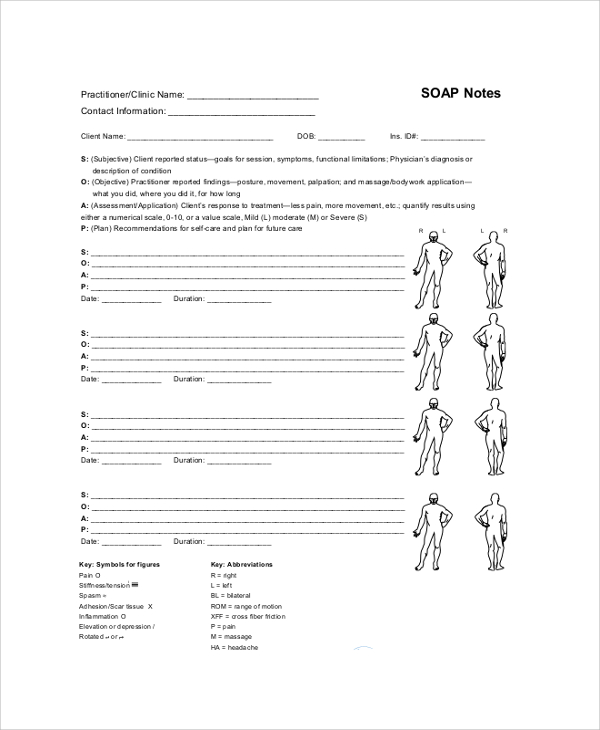
Sample Massage SOAP Note Example
This SOAP note example is designed specifically for massage therapists who identify and help you to get rid of your body pain. They are simple but enticing to look as they come with figures on which therapist marks the area and the treatment proposed for solving the same. You can also see more on Comprehensive Soap Note.
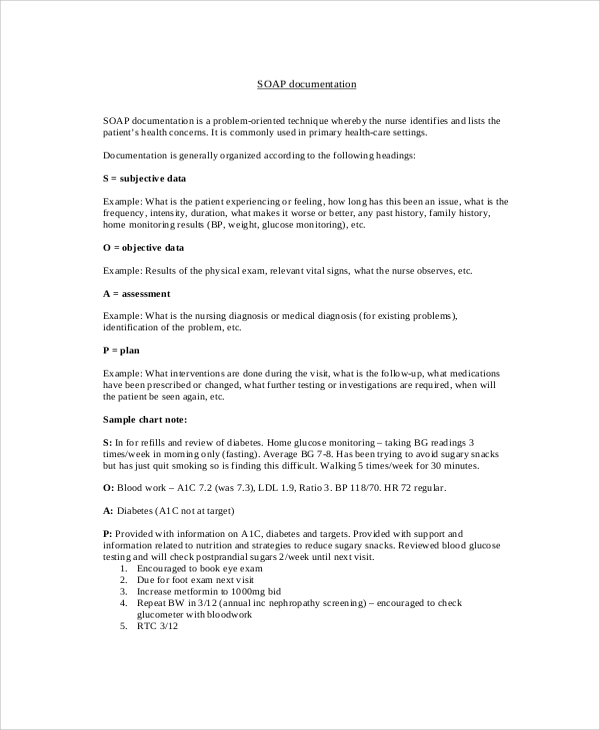
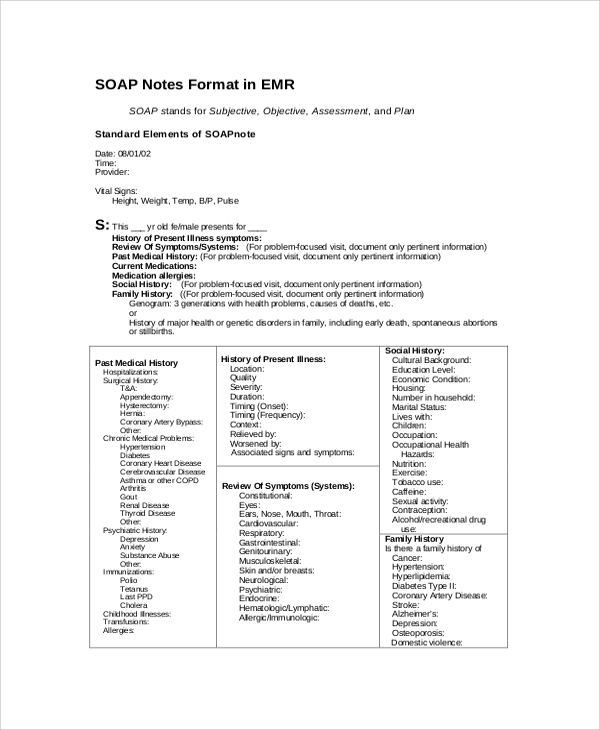
Example Of SOAP Notes Format
These notes as used as patient’s admission note as well recording the medical history and treatment measures. The format consists of the following heads- subjective, objective, assessment and plans. You can also see more on Sample SOAP Note.
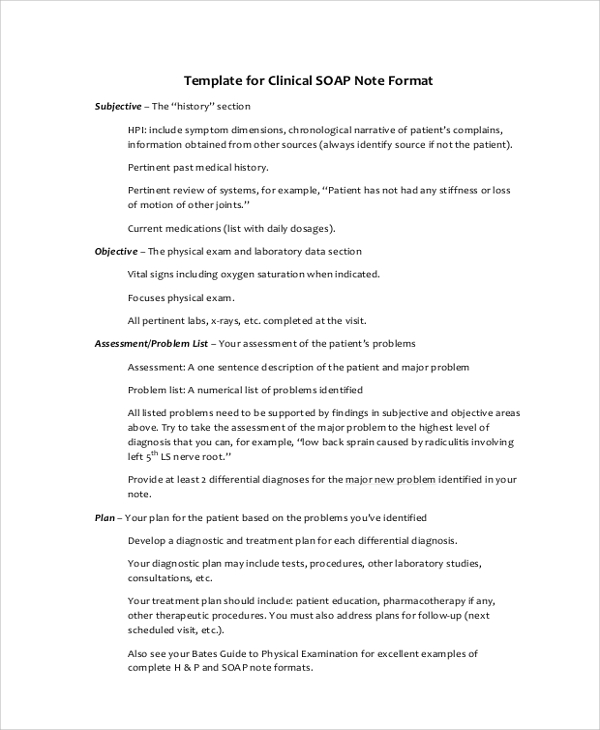
Sample Clinical SOAP Note Example
When you have to write down your observation about patients while having them around in the clinic, the best SOAP note you can make use of is the clinical SOAP note.
Tips For Writing SOAP Notes
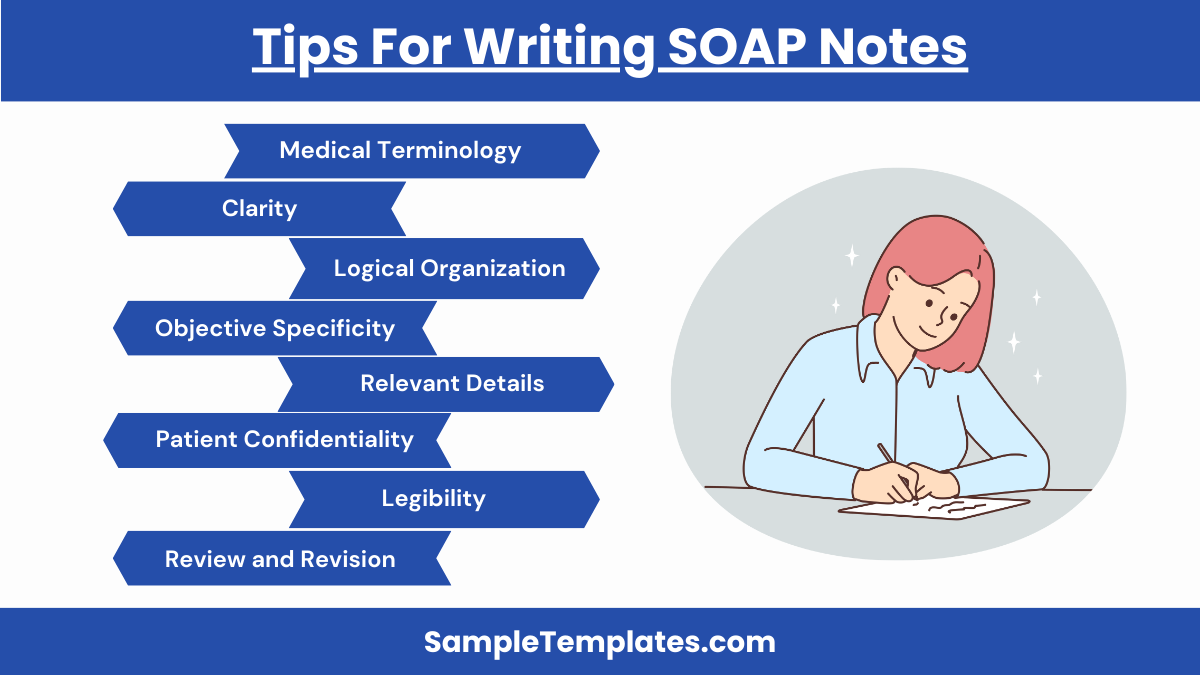
- Be Concise and Clear:
- Use clear, concise language to communicate information effectively. Avoid unnecessary jargon and lengthy descriptions.
- Use Medical Terminology Appropriately:
- Ensure that medical terminology is used correctly to maintain professionalism and clarity.
- Organize Information Logically:
- Follow the SOAP format strictly to keep information organized and easy to follow. Each section should be clearly defined and distinct.
- Be Objective and Specific:
- In the Objective section, only include factual, measurable data. Avoid subjective interpretations in this section. You can also see more on Student SOAP Note.
- Include Relevant Details:
- Ensure all pertinent information is included in the note. This may involve detailed descriptions of symptoms, physical findings, and test results.
- Keep it Legible and Professional:
- If handwritten, ensure your notes are legible. If typed, use a professional font and format. Always date and sign your notes.
- Maintain Patient Confidentiality:
- Follow all guidelines for protecting patient privacy. Do not include identifiable patient information inappropriately.
- Review and Revise:
- Take time to review your notes for accuracy and completeness. Make revisions as needed to ensure all necessary information is clearly documented. You can also see more on Blank Soap Note.
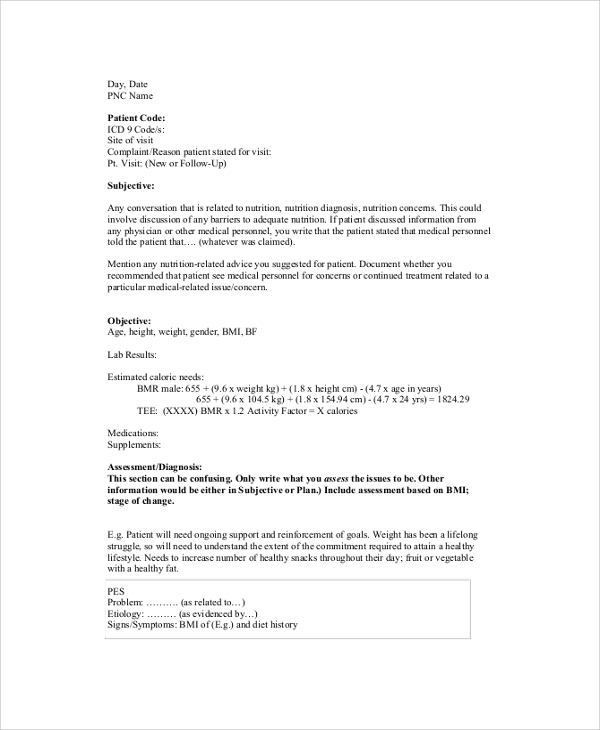
Sample PNC SOAP Note Example
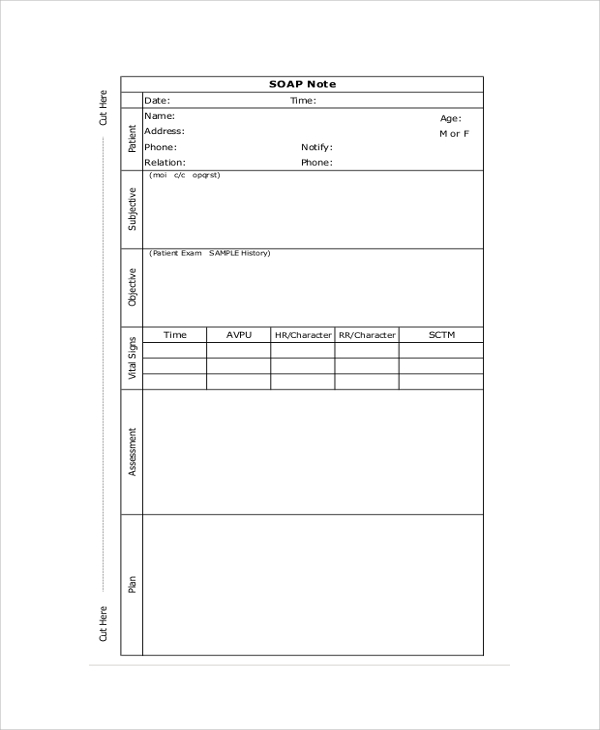
Sample SOAP Note Example
Printable SOAP Note Example
Benefits Of Using The SOAP Notes
Doctors and nurses encounter different patients in a single day. Keeping details about their diagnosis without jotting them down somewhere is not just difficult, rather impossible. This problem has been eased by the SOAP notes. Using these, you can systematically record every minute detail about the diagnosis under the heads- subjective and objective as well as prepare sample plans about the treatment and jot them down under the heads-assessment and plan.
These SOAP note samples listed above are highly in use by medical practitioners today. They come in appealing formats helping you to part away with the boring prescriptions. Using these will also help patients to understand their problem reading them once. Also, along with the SOAP note, you can get a thank you note printed too for the patients to make the therapy mood comfortable. So, do not forget to check for different Sample Thank You Notes along with the sample SOAP notes.
What is a SOAP note for dummies?
A SOAP note is a structured way for healthcare providers to document patient information, including Subjective (patient’s words), Objective (measurable data), Assessment (diagnosis), and Plan (treatment).
What goes under a in a SOAP note?
The “Assessment” section includes the healthcare provider’s diagnosis or clinical impressions based on the subjective and objective information, as well as any progress or changes in the patient’s condition. You can also see more on Medical Note.
Where do vitals go in a SOAP note?
Vitals, such as temperature, blood pressure, heart rate, and respiratory rate, are recorded in the Objective section of a SOAP note as they are measurable and observable data.
Where do goals go in a SOAP note?
Goals are typically outlined in the Plan section of a SOAP note. This includes the desired outcomes for the patient’s treatment and steps to achieve them.
What is a SOAP note for primary care?
A SOAP note for primary care is a detailed yet concise documentation method used by primary care providers to record patient interactions, diagnosis, treatment plans, and follow-up care systematically.
Are SOAP notes still used?
Yes, SOAP notes are still widely used in healthcare settings for their effectiveness in organizing patient information, ensuring continuity of care, and facilitating clear communication among healthcare providers.
In conclusion, this SOAP note provides a comprehensive overview of the patient’s current condition, diagnosis, and treatment plan. It ensures continuity of care by clearly documenting patient interactions and medical reasoning, aiding in effective communication among healthcare providers.
If you have any DMCA issues on this post, please contact us.
Related Posts
FREE 10+ Thank You Notes For Coworkers Samples in PDF
FREE 10+ Meeting Notes Samples in PDF
FREE 9+ Inpatient Progress Note Samples [ Psychiatric, Hospital, Complaint ]
FREE 10+ Note Taking Samples in PDF
FREE 10+ Credit and Debit Note Samples in PDF | MS Word
FREE 3+ Comprehensive Soap Note Samples in PDF
FREE 8+ Student SOAP Note Samples [ Medical, Pharmacy, Doctor ]
FREE 10+ Return Delivery Note Samples [ Product, Service, Electronic ]
FREE 3+ Car Sale Delivery Note Samples [ Transfer, Private, Vehicle ]
FREE 6+ Goods Delivery Note Samples [ Vehicle, Movement, Return ]
FREE 10+ Doctors Excuse Note Samples [ Office, Visit, Medical ]
FREE 5+ Discharge Summary Nursing Note Samples [ Progress, Patient, Home ]
FREE 6+ Labor and Delivery Note Samples [ Nurse, Progress, Admission ]
FREE 8+ Company Delivery Note Samples in PDF | DOC
FREE 5+ Material Delivery Note Samples in PDF