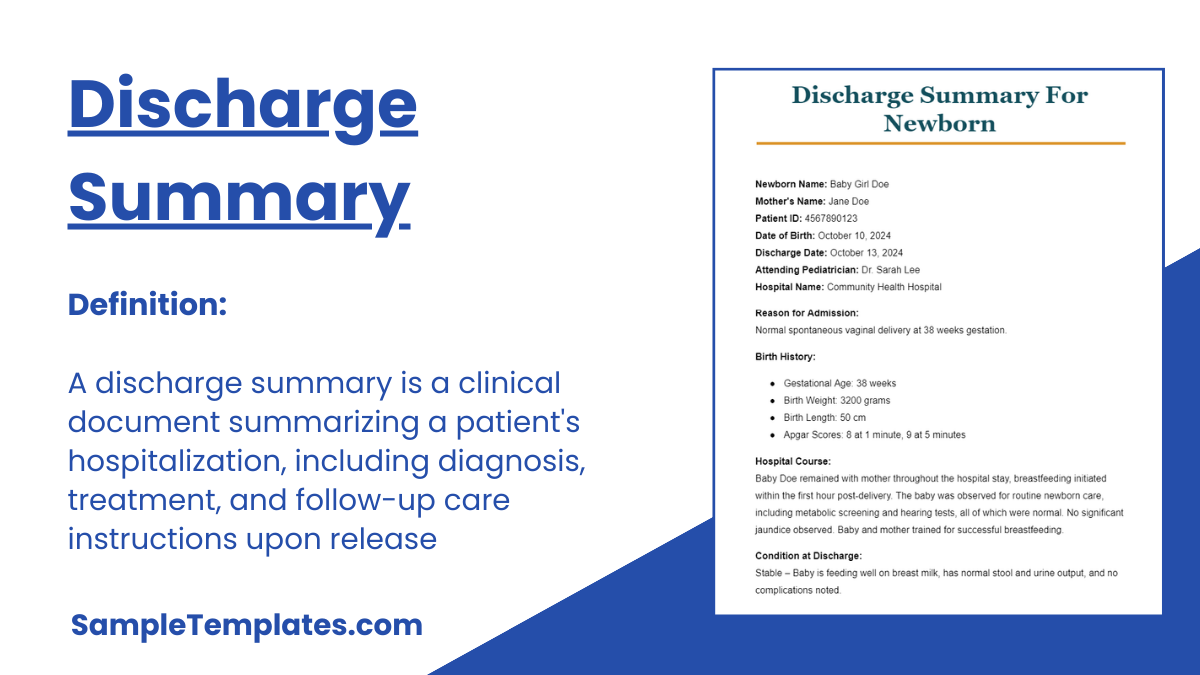
For patients who will give go home after extensive days in the hospital for treatment or surgery must have a discharge summary form to have the outline of all the procedures, operations, medications and therapy they went through. This Contract Summary tool is a requirement in some health insurances or social organizations in order to get the benefits in the said organization and in order to have the proof that they are really admitted and went some medical treatment.
All health facilities have their own discharge summary form sample; you can have your own made at Microsoft word program or just use the free sample template you can download in the internet. Discharge summary template will be the basis for having the guideline in summarizing all the medical management that a patient had in their admitted days.
Download Discharge Summary Bundle
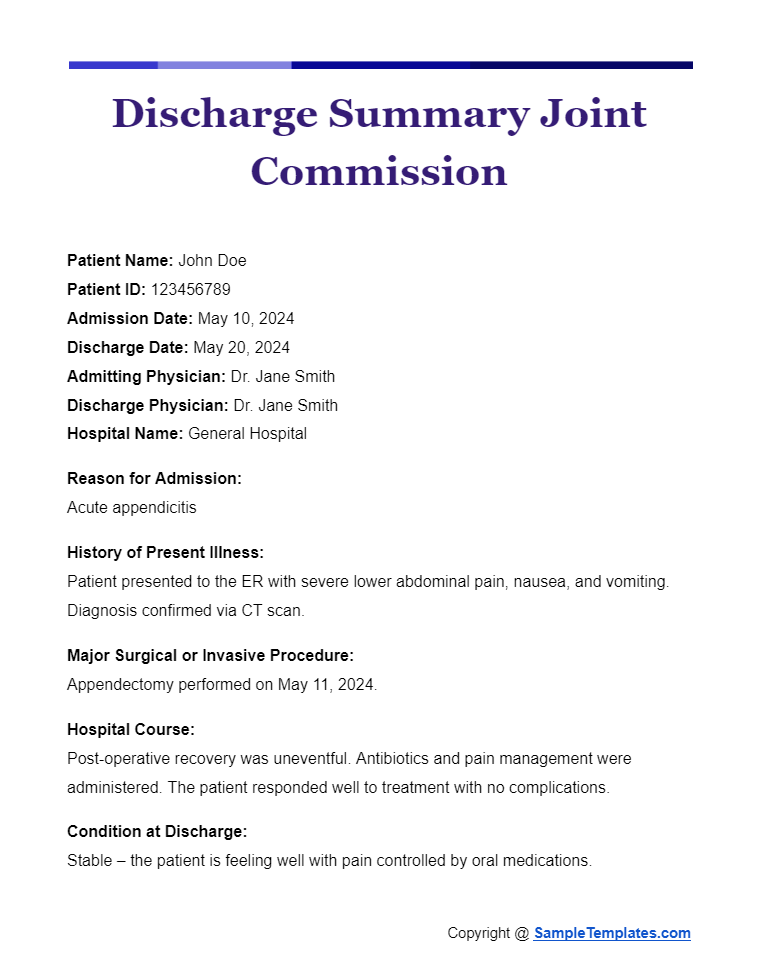
Discharge Summary Joint Commission
Patient Name: John Doe
Patient ID: 123456789
Admission Date: May 10, 2024
Discharge Date: May 20, 2024
Admitting Physician: Dr. Jane Smith
Discharge Physician: Dr. Jane Smith
Hospital Name: General Hospital
Reason for Admission:
Acute appendicitis
History of Present Illness:
Patient presented to the ER with severe lower abdominal pain, nausea, and vomiting. Diagnosis confirmed via CT scan.
Major Surgical or Invasive Procedure:
Appendectomy performed on May 11, 2024.
Hospital Course:
Post-operative recovery was uneventful. Antibiotics and pain management were administered. The patient responded well to treatment with no complications.
Condition at Discharge:
Stable – the patient is feeling well with pain controlled by oral medications.
Medications on Discharge:
- Acetaminophen 500 mg every 6 hours as needed for pain
- Amoxicillin 500 mg every 12 hours for 7 days
Allergies:
No known drug allergies
Follow-up Care:
Follow-up appointment with Dr. Jane Smith on May 30, 2024, at the General Hospital Outpatient Clinic.
Diet:
Regular diet as tolerated.
Activity:
No heavy lifting or strenuous activity for 4 weeks. Gradual return to normal activity as tolerated.
Instructions for Patient/Caregiver:
- Watch for signs of infection at the surgical site.
- Keep the wound dry and clean.
- Report any fever, increased pain, or redness around the incision site.
Summary of Counseling Provided to Patient/Caregiver:
The patient and caregivers were educated about the signs of potential complications, medication management, and the importance of follow-up care.
Copy to:
Primary Care Physician – Dr. Emily White
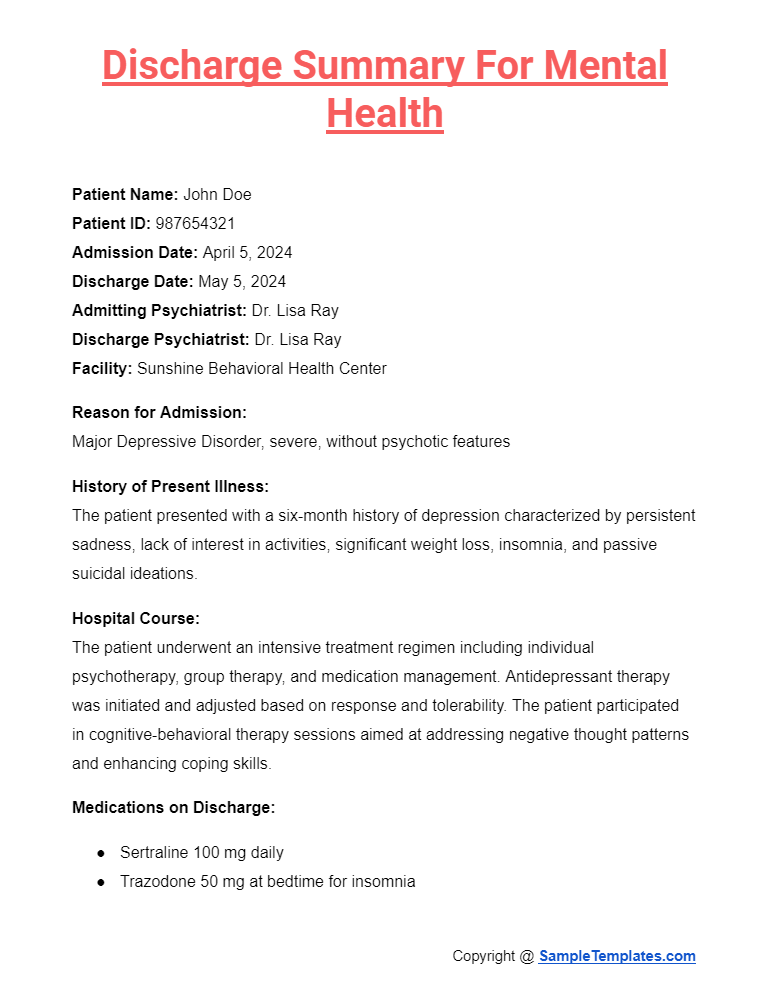
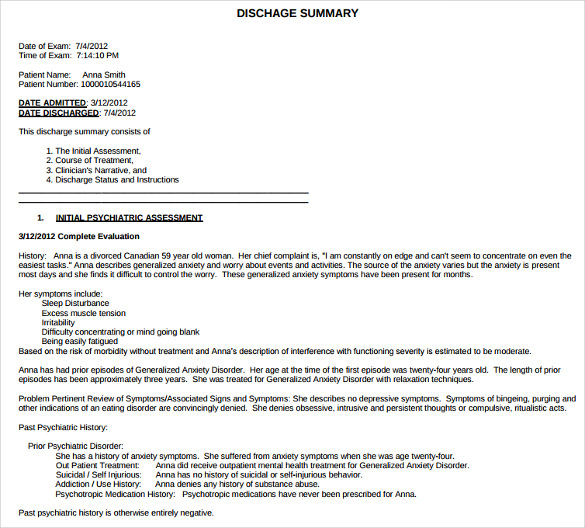
Discharge Summary for Mental Health
Patient Name: John Doe
Patient ID: 987654321
Admission Date: April 5, 2024
Discharge Date: May 5, 2024
Admitting Psychiatrist: Dr. Lisa Ray
Discharge Psychiatrist: Dr. Lisa Ray
Facility: Sunshine Behavioral Health Center
Reason for Admission:
Major Depressive Disorder, severe, without psychotic features
History of Present Illness:
The patient presented with a six-month history of depression characterized by persistent sadness, lack of interest in activities, significant weight loss, insomnia, and passive suicidal ideations.
Hospital Course:
The patient underwent an intensive treatment regimen including individual psychotherapy, group therapy, and medication management. Antidepressant therapy was initiated and adjusted based on response and tolerability. The patient participated in cognitive-behavioral therapy sessions aimed at addressing negative thought patterns and enhancing coping skills.
Medications on Discharge:
- Sertraline 100 mg daily
- Trazodone 50 mg at bedtime for insomnia
Allergies:
No known drug allergies
Condition at Discharge:
Much improved. The patient reports a significant reduction in depressive symptoms and denies any current suicidal ideation.
Psychosocial Interventions:
- Cognitive Behavioral Therapy
- Supportive psychotherapy
- Stress management sessions
Follow-up Care:
Follow-up appointment with outpatient psychiatrist Dr. Emily White on May 15, 2024, at Community Mental Health Clinic. The patient is also recommended to continue weekly sessions with a licensed therapist.
Safety Plan:
The patient and care team developed a safety plan including identifying warning signs of relapse, coping strategies, and emergency contacts.
Instructions for Patient/Caregiver:
- Continue medication as prescribed without interruption.
- Attend all scheduled therapy sessions.
- Engage in daily physical activity and social interactions as tolerated.
Summary of Counseling Provided to Patient/Caregiver:
Extensive counseling was provided regarding medication adherence, recognizing signs of relapse, and utilizing support systems. Education was also provided about the importance of ongoing therapy and lifestyle modifications supporting mental health.
Copy to:
- Primary Care Physician
- Outpatient Psychiatrist
- Therapist
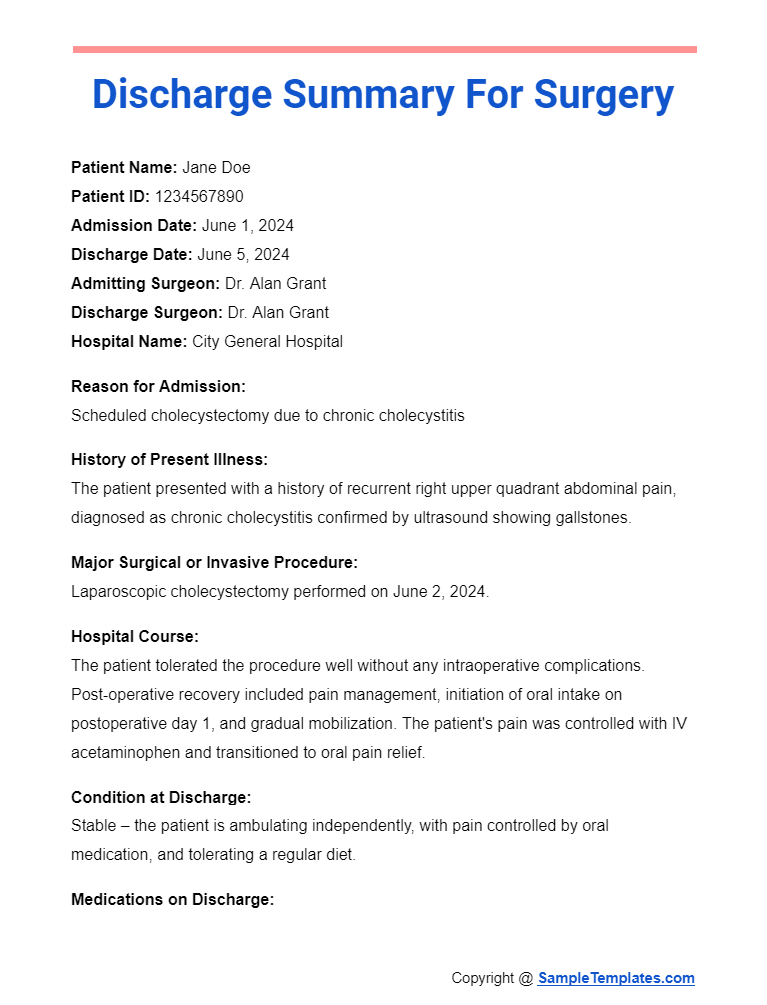
Discharge Summary for Surgery
Patient Name: Jane Doe
Patient ID: 1234567890
Admission Date: June 1, 2024
Discharge Date: June 5, 2024
Admitting Surgeon: Dr. Alan Grant
Discharge Surgeon: Dr. Alan Grant
Hospital Name: City General Hospital
Reason for Admission:
Scheduled cholecystectomy due to chronic cholecystitis
History of Present Illness:
The patient presented with a history of recurrent right upper quadrant abdominal pain, diagnosed as chronic cholecystitis confirmed by ultrasound showing gallstones.
Major Surgical or Invasive Procedure:
Laparoscopic cholecystectomy performed on June 2, 2024.
Hospital Course:
The patient tolerated the procedure well without any intraoperative complications. Post-operative recovery included pain management, initiation of oral intake on post-operative day 1, and gradual mobilization. The patient’s pain was controlled with IV acetaminophen and transitioned to oral pain relief.
Condition at Discharge:
Stable – the patient is ambulating independently, with pain controlled by oral medication, and tolerating a regular diet.
Medications on Discharge:
- Acetaminophen 500 mg every 6 hours as needed for pain
- Ibuprofen 400 mg every 8 hours as needed for pain
Allergies:
No known drug allergies
Follow-up Care:
Follow-up appointment with Dr. Alan Grant on June 12, 2024, at City General Hospital Surgical Clinic.
Diet:
Resume normal diet as tolerated.
Activity:
Avoid lifting objects heavier than 10 pounds for 4 weeks. Gradual increase in daily activities as tolerated.
Instructions for Patient/Caregiver:
- Monitor the incision site for signs of infection (redness, swelling, discharge).
- Keep the incision dry and clean.
- Report any symptoms of fever, persistent pain, or nausea.
Summary of Counseling Provided to Patient/Caregiver:
The patient and caregiver were educated about post-operative care, signs of complications, medication management, and the importance of follow-up visits.
Copy to:
- Primary Care Physician
- Outpatient Surgical Team
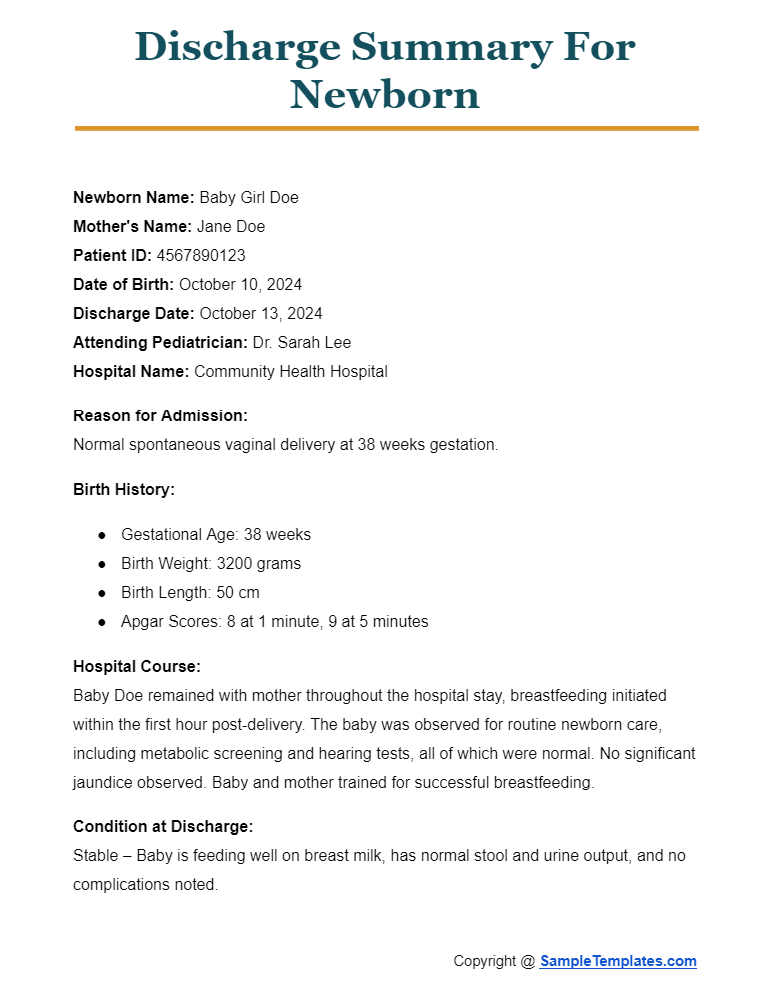
Discharge Summary for Newborn
Newborn Name: Baby Girl Doe
Mother’s Name: Jane Doe
Patient ID: 4567890123
Date of Birth: October 10, 2024
Discharge Date: October 13, 2024
Attending Pediatrician: Dr. Sarah Lee
Hospital Name: Community Health Hospital
Reason for Admission:
Normal spontaneous vaginal delivery at 38 weeks gestation.
Birth History:
- Gestational Age: 38 weeks
- Birth Weight: 3200 grams
- Birth Length: 50 cm
- Apgar Scores: 8 at 1 minute, 9 at 5 minutes
Hospital Course:
Baby Doe remained with mother throughout the hospital stay, breastfeeding initiated within the first hour post-delivery. The baby was observed for routine newborn care, including metabolic screening and hearing tests, all of which were normal. No significant jaundice observed. Baby and mother trained for successful breastfeeding.
Condition at Discharge:
Stable – Baby is feeding well on breast milk, has normal stool and urine output, and no complications noted.
Feeding:
Exclusive breastfeeding on demand, approximately every 2-3 hours.
Medications:
Vitamin D supplementation 400 IU daily.
Allergies:
No known allergies.
Follow-up Care:
- Pediatric follow-up appointment with Dr. Sarah Lee on October 20, 2024, at Community Pediatric Clinic.
- Schedule further routine immunizations per pediatric immunization guidelines.
Home Care Instructions:
- Continue breastfeeding on demand.
- Monitor for signs of dehydration (fewer than six wet diapers in 24 hours).
- Check daily for any signs of jaundice.
- Keep the newborn warm and practice safe sleeping guidelines.
Safety Measures:
- Follow SIDS prevention guidelines: Place the baby on her back to sleep, use a firm sleep surface, keep soft objects away from the sleeping area.
- Ensure smoke-free environment.
Instructions for Emergency:
- Contact pediatrician if the baby shows signs of lethargy, refuses to feed, has a fever above 100.4°F, or if there are any concerns about breathing.
Summary of Counseling Provided to Parent(s):
Parents were educated about newborn care including feeding, sleeping, hygiene, and signs of illness. They were also informed about postpartum care for the mother.
Copy to:
- Primary Care Pediatrician
- Obstetrician
Browse More Templates On Discharge Summary
Hospital Discharge Summary Format Word
Patient Discharge Summary Template
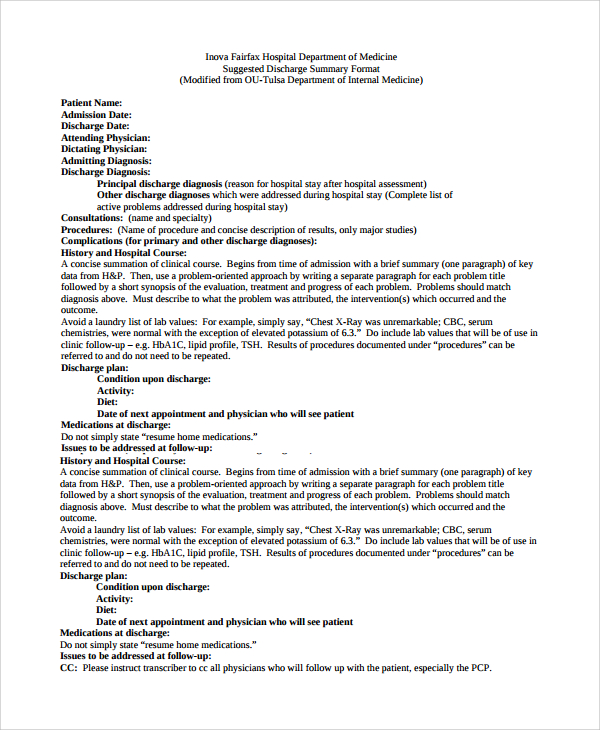
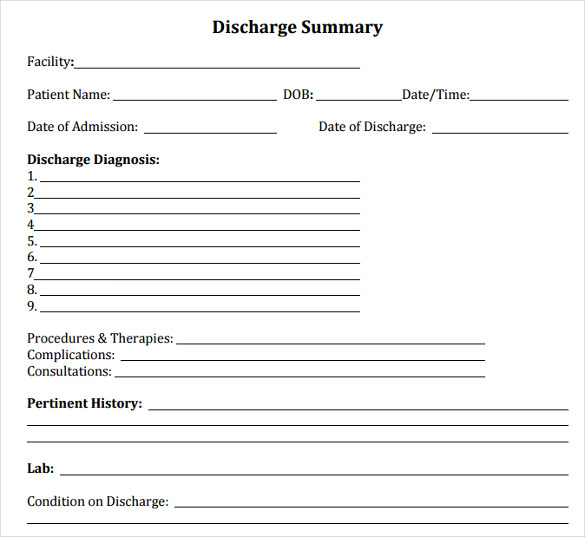
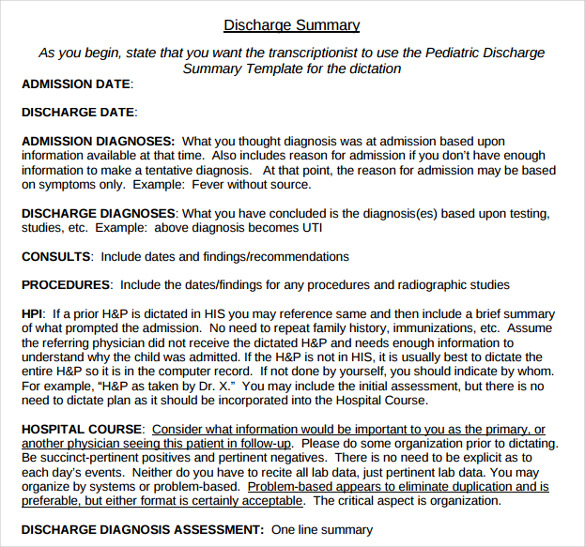
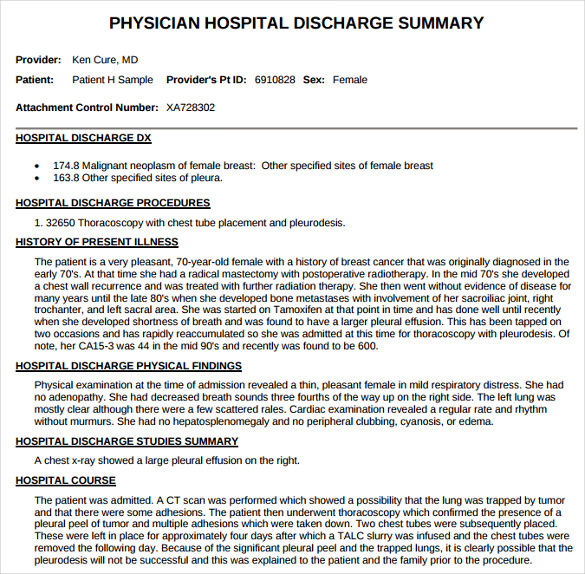
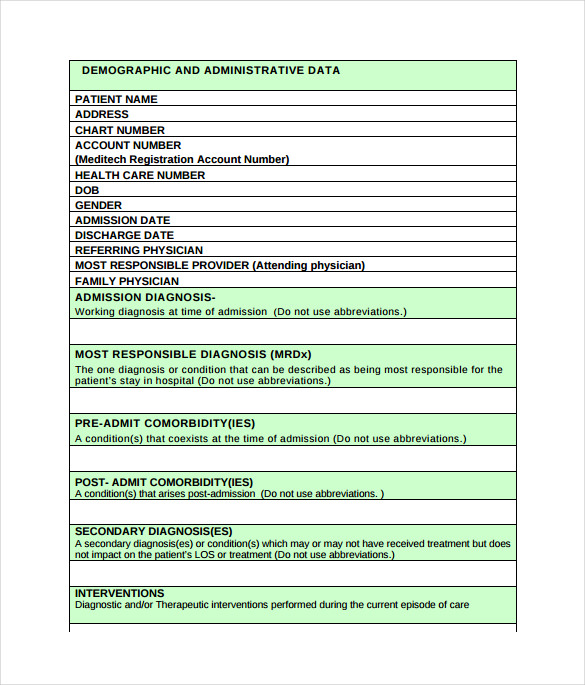
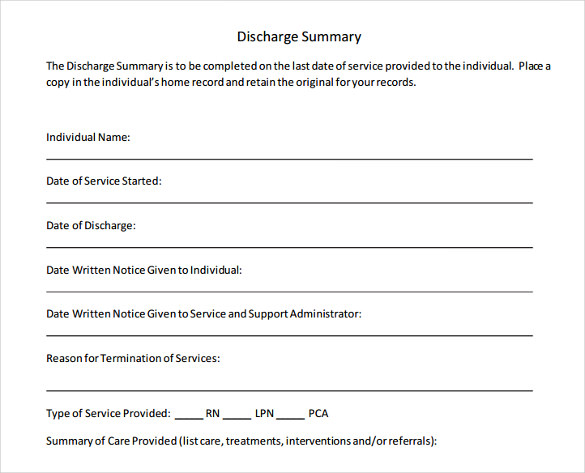
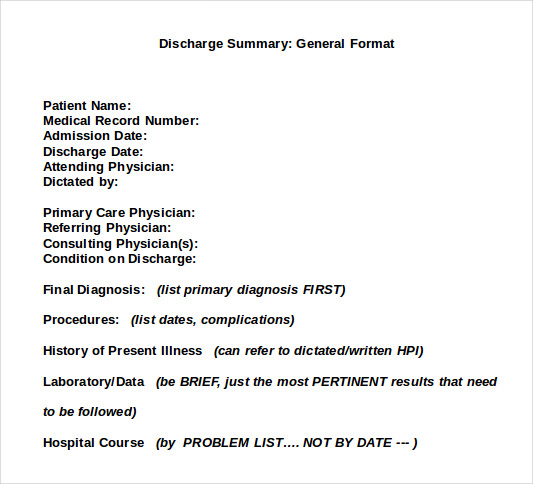
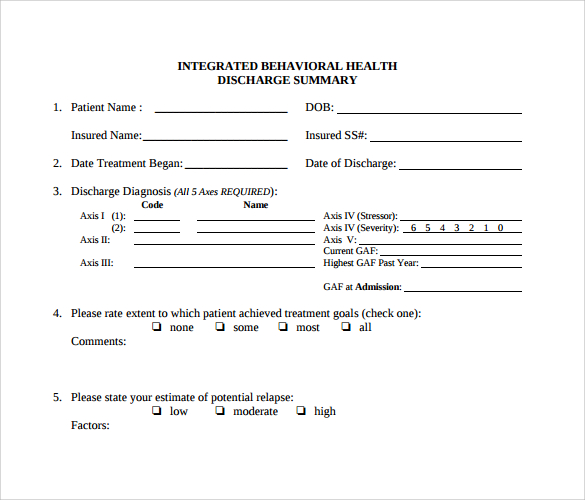
The Suggested Discharge Summary Template is one of the most important and crucial templates that you can use in any medical institutions ranging from hospitals, clinics, nursing homes, and others. All of these templates contain details about admission and discharge dates, names of physicians involved in the treatment, initial and final diagnoses reports sample, and other key factors related to operations and medical procedures performed.
Discharge Summary Sample PDF
What Should a Discharge Summary Include?
A discharge summary is a critical document that outlines a patient’s hospital stay and the care they received. Here are the key elements it should include:
- Patient Information: Name, patient ID, date of birth, and any other relevant identifiers.
- Admission and Discharge Dates: The specific dates the patient was admitted and discharged from the facility.
- Admitting and Discharge Physician: Names and specialties of the physicians responsible for the patient’s care upon admission and at discharge.
- Hospital Name and Department: The name of the hospital and specific department or unit where the patient was treated.
- Reason for Admission: A brief statement on why the patient was admitted, including primary diagnosis.
- Hospital Course: A summary of the treatment the patient received, including:
- Surgeries and Procedures: Dates and descriptions of any surgical procedures or significant medical interventions.
- Medication Changes: Any changes in medication during the hospital stay.
- Consultations: Information about any specialist consultations.
- Significant Findings: Results of important tests or diagnostics.
- Condition at Discharge: The patient’s health status at the time of discharge, noting improvements or complications.
- Medications on Discharge: A list of medications prescribed at discharge, including dosages and frequency.
- Allergies: List of known drug allergies.
- Follow-up Care: Details about:
- Follow-up Appointments: Time, date, and with whom the follow-up appointments are scheduled.
- Tests and Procedures: Any scheduled tests or procedures needed after discharge.
- Therapies: Information on any continuing therapy, such as physical, occupational, or speech therapy.
- Dietary and Activity Instructions: Specific guidelines on diet and physical activity limitations or recommendations.
- Specific Instructions for Care: Detailed instructions for care related to the patient’s condition, including how to care for wounds, manage pain, and recognize potential complications.
- Emergency Instructions: Guidance on what to do and who to contact in case of an emergency post-discharge.
- Summary of Counseling Provided: A brief description of the counseling and education provided to the patient and their caregiver about the condition and its management.
- Copy To: Listing of other healthcare providers or facilities to whom copies of the discharge summary should be sent, to ensure continuity of care.
The discharge summary serves as a bridge between hospital care and follow-up care, ensuring that all subsequent caregivers are fully informed about the patient’s hospitalization and ongoing care needs.
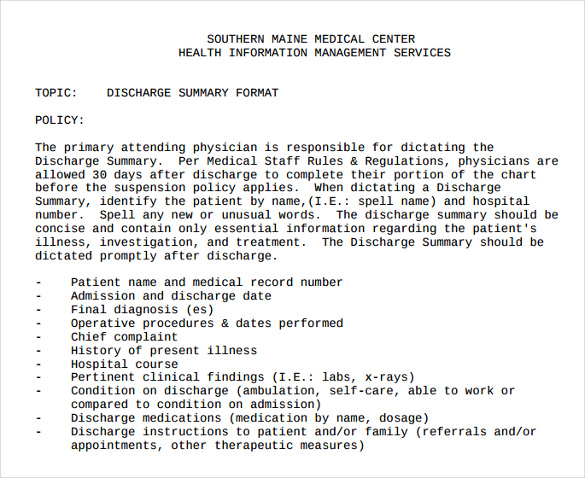
Discharge Summary Format
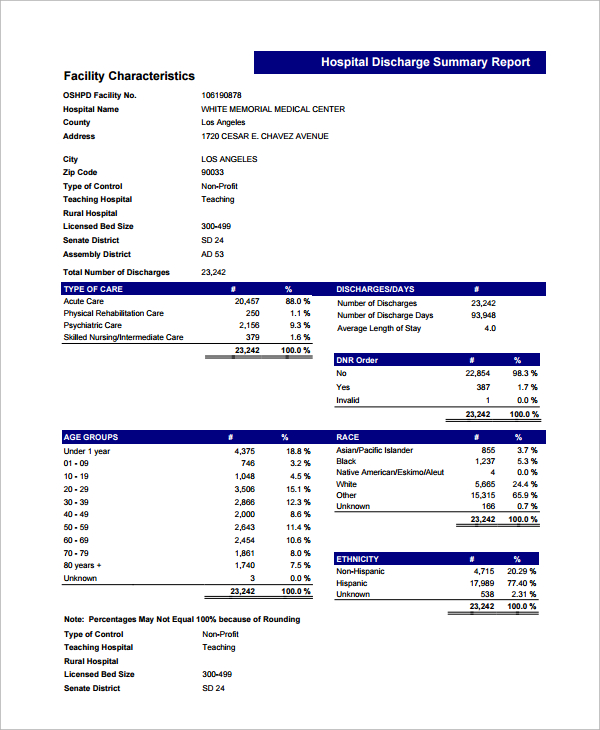
The Hospital Discharge Summary Report Template is created, drafted, and designed to help you sample note down a detailed overview of a patient’s hospitalization. Beginning with all the details that have been mentioned at the time of admission and details about the things that have happened till discharge are listed in this template.
Discharge Summary Format PDF
The Nursing Home Discharge Summary Template is designed and crafted to help you enlist the essential elements of the discharge summary in detail. All of these templates enable you to provide various details about the hospitalization including the Final diagnoses performed, brief description of reason for admission, brief medicinal course evaluation, and condition of patient at the time of discharge, and other vital factors.
Benefits of Discharge Summary
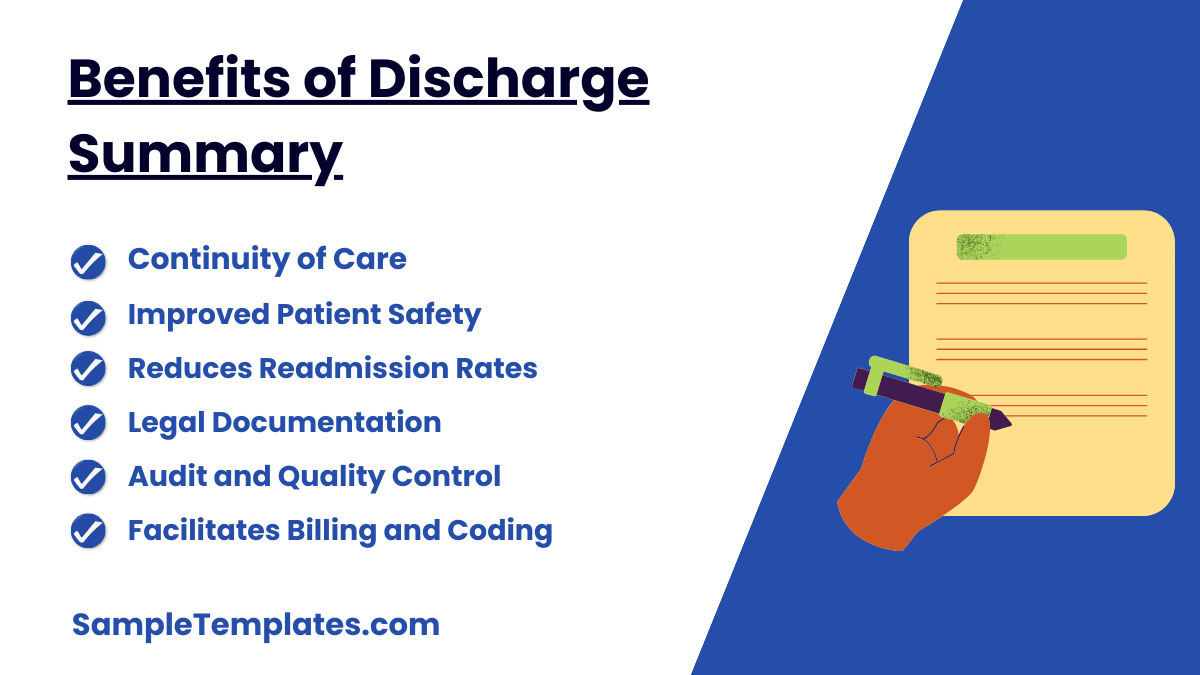
A discharge summary is an essential document in the continuum of patient care, serving as a critical communication tool that benefits both healthcare providers and patients. Here are the main benefits of a discharge summary:
- Continuity of Care: It provides a comprehensive record of a patient’s hospital stay, including diagnosis, treatment, and care provided, which is crucial for subsequent caregivers. This ensures that everyone involved in the patient’s care after discharge is informed and can make well-coordinated decisions.
- Improved Patient Safety: By detailing the patient’s condition at discharge, medications prescribed, follow-up needs, and potential complications, the summary helps prevent medical errors and adverse events post-discharge.
- Reduces Readmission Rates: Effective discharge summaries can help reduce hospital readmissions by ensuring that follow-up care is appropriately managed, complications are monitored, and transitional care is well-coordinated.
- Enhances Patient Understanding and Compliance: The summary helps patients and caregivers understand the care instructions, medications, and follow-up appointments, which can increase adherence to treatment plans and enhance recovery outcomes.
- Legal Documentation: It acts as a legal document that can be referred back to in case of disputes or claims regarding the patient’s treatment and hospital stay. It records the healthcare provided and the rationale behind treatment decisions.
- Audit and Quality Control: Discharge summaries can be reviewed for quality assurance purposes, helping healthcare institutions monitor and improve their care processes.
- Facilitates Billing and Coding: Accurate discharge summaries aid in the coding and billing process by providing clear documentation of diagnoses and treatments, which is necessary for reimbursement from insurance providers.
- Supports Public Health Reporting: Information from discharge summaries can be used for public health monitoring, research, and reporting, helping to track health trends and outcomes.
- Efficient Use of Healthcare Resources: By providing clear post-discharge instructions and follow-up care plans, discharge summaries help optimize the use of healthcare resources, preventing unnecessary emergency visits and optimizing outpatient care.
Overall, the discharge summary is a pivotal document that enhances communication among healthcare providers, supports patient care continuity, and contributes to the overall health system’s efficiency and effectiveness.
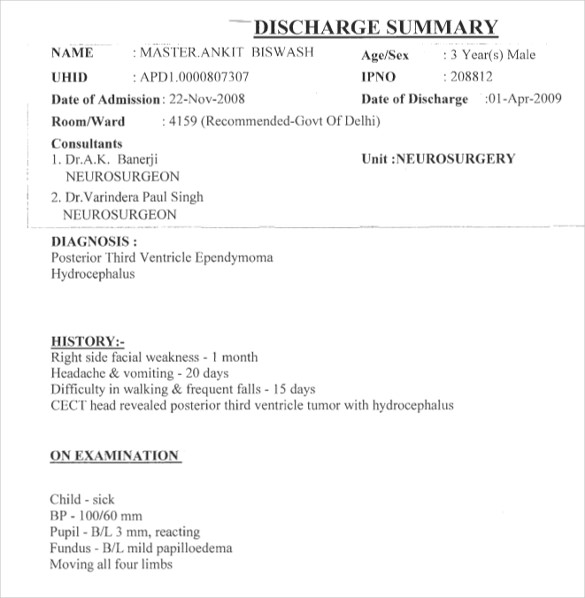
Discharge Summary Example
Discharge Summary Sample
Hospital Discharge Summary Format PDF
Hospital Discharge Summary Template
Discharge Summary Format PDF Download
Importance Of Discharge Summary
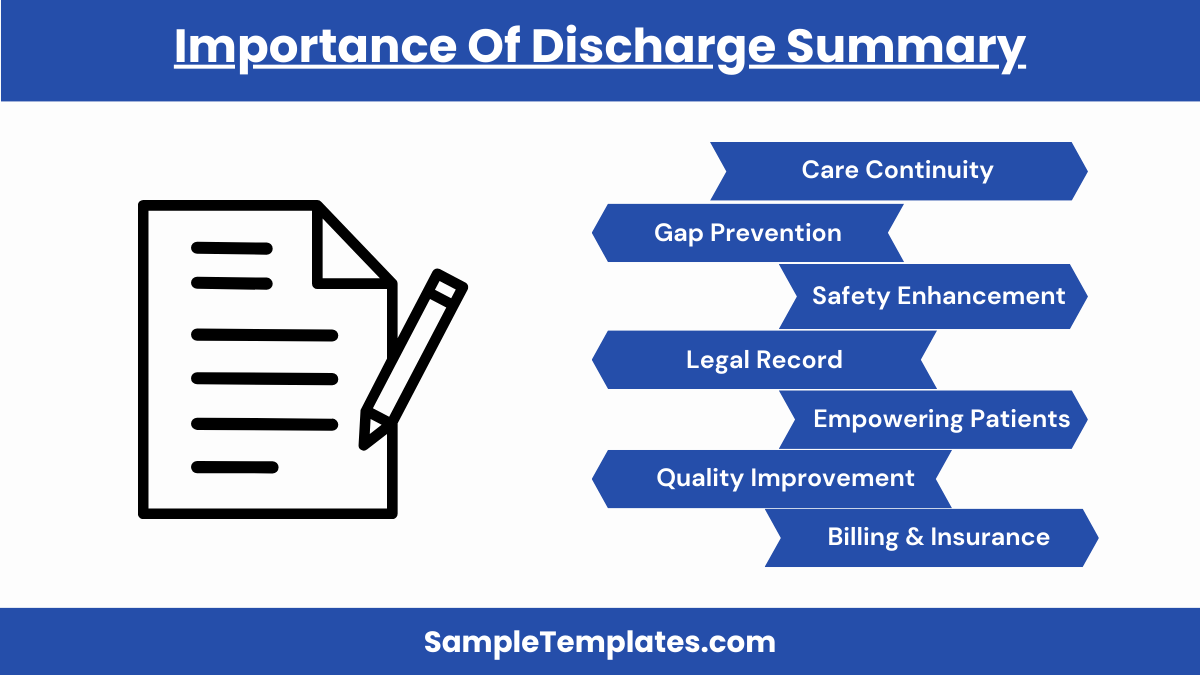
The discharge summary holds a critical role in healthcare, bridging inpatient care and community-based or follow-up care. It’s not only a key document for continuity of care but also for ensuring the safety and well-being of patients post-discharge. Here’s why the discharge summary is so important:
- Continuity of Care: The discharge summary provides a comprehensive overview of a patient’s hospital stay, including diagnosis, treatment administered, and care outcomes. This documentation ensures that subsequent healthcare providers are well-informed and can continue care seamlessly, adjusting treatments as necessary based on a clear history.
- Prevents Gaps in Care: Detailed summaries include follow-up plans, medication instructions, and potential signs of complications, which are essential for preventing gaps in care. These instructions help ensure that patients receive appropriate and timely medical attention after leaving the hospital.
- Enhances Patient Safety: The summary helps prevent medication errors and adverse events. For instance, it lists new medications, changes in existing prescriptions, and potential drug interactions, critical information that can prevent harmful mistakes.
- Reduces Hospital Readmissions: A clear, detailed discharge plan can help minimize the risk of readmission by ensuring patients and caregivers understand the care instructions, recognize the warning signs of potential complications, and know when to seek medical advice.
- Legal Documentation: It serves as a legal record of the care provided and the patient’s health status at discharge. This can be crucial for addressing any legal inquiries or disputes about the patient’s treatment.
- Patient Empowerment: By receiving a clear summary of their hospital stay and ongoing care instructions, patients and caregivers are better equipped to manage their health, leading to improved outcomes and patient satisfaction.
- Quality Improvement: Healthcare providers can use discharge summaries to evaluate the quality of care delivered, identify patterns, and implement improvements. It also aids accreditation and compliance with healthcare standards and regulations.
- Facilitates Effective Communication: It ensures that all health professionals involved in the care continuum, from primary care doctors to specialists and outpatient caregivers, receive the same information, promoting effective communication and collaborative care.
- Billing and Insurance: The document supports accurate billing and insurance claims, providing necessary details that justify patient treatments and hospital stays.
Overall, the discharge summary is fundamental for a well-functioning healthcare system, contributing significantly to patient outcomes, the efficacy of follow-up care, and the overall safety and satisfaction of patients.
Discharge Summary
Discharge Paper Format
Hospital Discharge Slip
Discharge Summary Report PDF
Hospital Discharge Summary Example
Why You Must Use These Readymade Templates?
One of the biggest challenges that most of the medical institutions face while managing the records and details of the patients they’ve provided treatments to is that they don’t follow a universal format to maintain a streamlined entries. You can also see Case Summary
All of the these templates can assist in applying a universal format while enlisting details about the patients, their treatments, doctors aligned to them, operations and procedures performed during the treatment, medication list on discharge and other such details to ensure that the hospital staff has a complete record of all the things that has been performed before the patient gets discharged.
Some of the specialized discharge templates enable the hospital staff or data management Plan teams to enlist significant findings and test results in detail for ensuring minimal disputes at the time of discharge. All of these templates can be customized to enlist medicinal plan sample, follow-up appointments details, and emergency contact details of the physicians aligned to help you experience the best medical treatment.
How to Write a Discharge Summary?
A discharge summary is a medical document that summarizes a patient’s hospital stay. It typically includes the patient’s medical history, diagnosis, treatment, medications, and follow-up recommendations. Write it in a clear, concise, and structured format, focusing on essential information to ensure proper post-hospital care.
What Should Be Included in a Hospital Discharge Summary?
A hospital discharge summary should include the patient’s medical history, diagnosis, treatment received during the hospital stay, prescribed medications, follow-up instructions, and any relevant test results.
What is a discharge summary for a claim?
A discharge summary for a claim is a document detailing the closure of an insurance claim. It outlines the final settlement, terms, and any remaining obligations or actions needed to complete the claim process.
What is a discharge summary in OT?
In occupational therapy (OT), a discharge summary is a document summarizing a patient’s progress, goals achieved, treatment interventions, and recommendations upon completing their OT program. It aids in tracking patient outcomes and future care planning.
What is a discharge summary nursing note?
A discharge summary nursing note is a document created by a nurse when a patient is discharged from a healthcare facility. It includes essential details about the patient’s condition, care provided, and post-discharge instructions.
What is discharge synopsis?
A discharge synopsis is a concise document summarizing key details of a patient’s hospital stay. It typically includes medical history, diagnosis, treatment, medications, and post-discharge instructions for continuity of care.
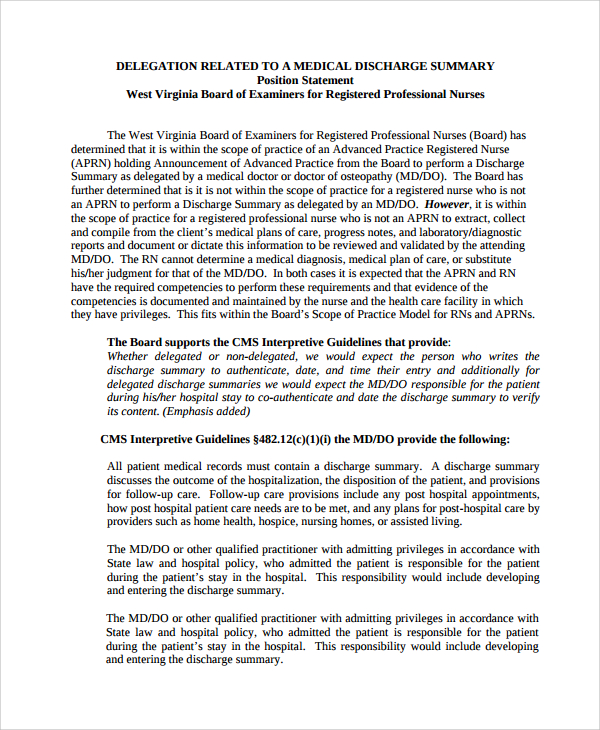
Who will prepare discharge summary?
A discharge summary is typically prepared by a medical team, including physicians, nurses, and healthcare providers who have been involved in a patient’s care during their hospital stay.
In conclusion, this discharge summary encapsulates the patient’s medical journey, treatment, and ongoing care plan. It serves as a comprehensive record to guide post-discharge care and ensure continuity. The healthcare team remains committed to the patient’s well-being, and we appreciate collaboration in sustaining a healthy and supported recovery.
If you have any DMCA issues on this post, please contact us
Related Posts
FREE 31+ Sample Business Plan Templates in Google Docs | MS Word | Pages | PDF
FREE 22+ Sample Training Plan Templates in Google Docs | MS Word | Pages | PDF
FREE 32+ Cost Analysis Samples in PDF | MS Word | Excel
FREE 10+ Stakeholder Analysis Samples in Google Docs | MS Word | Pages | PDF
FREE 11+ Sample Job Analysis Templates in Excel | Google Docs | MS Word | Pages | PDF
FREE 16+ Business Analysis Samples in MS Word | Google Docs | Pages
FREE 6+ Sample Printable Employee Handbook Templates in PDF | Google Docs | Pages | MS Word
FREE 13+ Policy and Procedure Templates in PDF
FREE 13+ Statement of Work Templates in Google Docs | MS Word | Pages | PDF
FREE 18+ Sample Price List Templates in PDF | MS Word | Pages | Google Docs | Google Sheets | Numbers | MS Excel | PSD | AI | Publisher
FREE 9+ Training Log Templates in PDF | MS Word
FREE 17+ Sample Downloadable Sales Agreement Templates in Google Docs | MS Word | Pages | PDF
FREE 13+ Sample Purchase Agreement Templates in PDF | MS Word | Pages
FREE 20+ Sample Buy Sell Agreement Templates in PDF | MS Word | Google Docs | Pages
FREE 18+ Sample Consignment Agreement Templates in Google Docs | MS Word | Pages | PDF