Nurses are known as the backbone of the medical community as they take care of the patients during the doctors’ absence and are required to submit an informative history of care and injury by accomplishing a nursing report. It is necessary for a nurse to complete their nursing reports because doctors utilize them to keep track of the patient’s progress report to determine whether their treatment plans are effective or not once it has been prescribed. With a nursing report sheet or template, nurses will be able to easily keep track of the progress of each of their patients.
3+ Nurse Report Sheet Samples
1. Nurse Report Sheet for Newbies
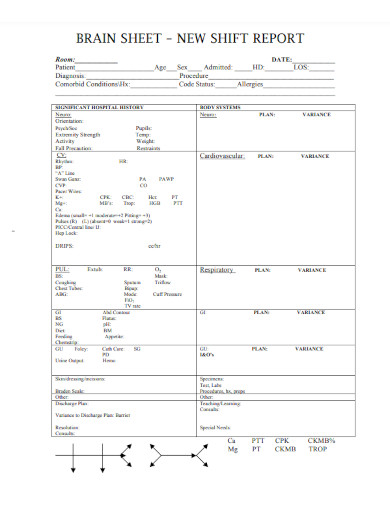
2. Nurse New Shift Report Sheet
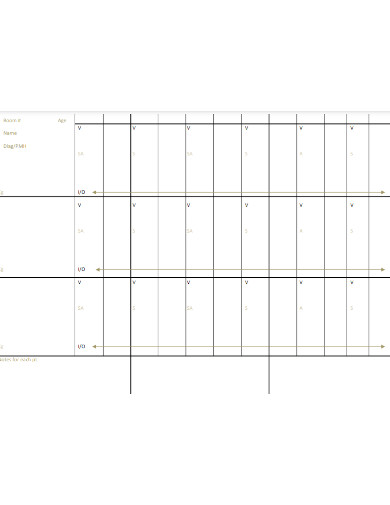
3. Nursing Report Sheet
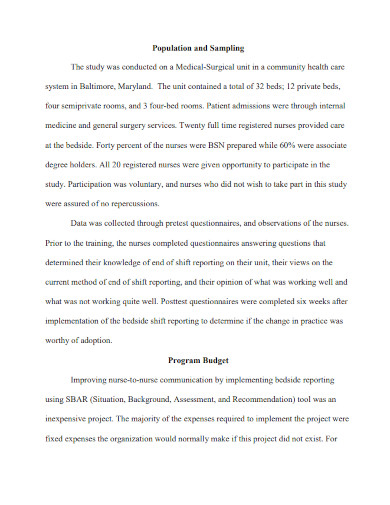
4. Nurse-To-Nurse End of Shift Report
What Is a Nurse Report Sheet?
A nursing report sheet is a ready-to-use template utilized by nurses at the beginning of their shifts when they get another nurse’s report who is ending their shift. This report worksheet helps nurses in keeping track of their patient’s progress which also contains critical information about their patient’s medical history, diagnosis, allergies, consults, their attending doctors, lab results, vital signs, medication times, and more.
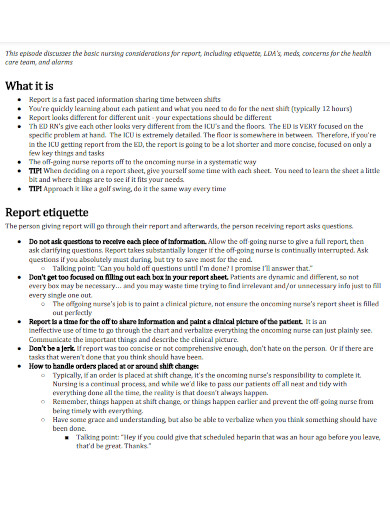
How to Write a Nursing Report
Producing an effective nursing report enables a smoother shift transition for the nurses while efficiently monitoring the progress of their patients. A nursing report sheet is used to access a shift report which contains valuable information about every patient under their care. The report sheet provides details in each patient’s name, the reason for their admission, and other relevant information such as medications for the day, nutritional status, lab reports, code status, vital signs, and more.
Step 1: Collect Subjective Evidence from a Patient
Once you have recorded the date, time, and the patient’s name, you can start your nursing progress note by collecting subjective evidence which includes the patient’s pain level, the reason for their admission, and other concerns they might have. If in the proper situation, try asking any family member or friend escorting the patient if they have observed anything related to the patient’s health.
Step 2: Keep a Record of the Information and your Assessment
After communicating with your patient, collect objective data to put in your notes which includes the patient’s observable symptoms, vitals, and test results. You also have to include your assessment which refers to your observation of the patient’s appearance, symptoms, and attitude after their medication was prescribed when their admission started.
Step 3: Construct a Care Plan
The care plan on your progress notes contains the course plan that the doctor has created to provide the patient. If the patient is going to take an MRI scan, it should be mentioned in your notes or report. You also have to include important and relevant information about the patient’s reaction to your healthcare plan.
Step 4: Include Additional Notes for Additional Facts
This section includes a variety of information but it mostly contains details on any additional facts related to the care that the patient has received during a nurse’s shift. It includes details on the time they administered medication to the patient, requests they might have, and other observations of their condition.
FAQs
Why do nurses utilize nursing report sheets?
As a nurse, a nursing report sheet enables you to keep track of telephone orders you received from a doctor, keep track of intake and output, keep track of blood sugars and insulin coverage, contain nursing notes to remind you of your tasks, and keeps notes of things you want to remind the next shift.
What are the elements included in a nursing progress report?
A nursing progress report includes the date and time when the report was written, the patient’s name, the doctor and nurse’s name, a general description of the patients, the reason for their visit or admission, vital signs and initial health assessment, diagnosis and care plan, their response to care, and additional observations.
What are the benefits of using a nursing report sheet?
With a nursing report sheet, both doctors and nurses can have quick access to their patient’s information, keep track of the tasks a nurse has to complete before the end of their shift, helps in differentiating the diagnosis and histories of each patient, and helps in more accurate charting.
A nursing report sheet is a template that nurses can readily use to keep track of their patient’s progress as well as their observations during the patient’s treatment. This document contains essential information about their patients such as their diagnosis, medical history, details on their attending doctor, medical consultations, individual treatment plan, and other observations on the patient’s treatment response that a nurse has obtained during their shift.
Related Posts
FREE 7+ Nursing Staffing Plan Samples in MS Word Google Docs ...
FREE 59+ Incident Report Formats in PDF MS Word | Google Docs
FREE 10+ Nurses Meeting Minutes Samples in PDF DOC
FREE 9+ Daily Report Samples in PDF MS Word
FREE 17+ Sample Handover Reports in PDF MS Word | Google ...
FREE 10+ Career Investigation Report Samples in PDF DOC
FREE 10+ Nurses Notes Samples in PDF
FREE 12+ Sample Testing Reports in PDF MS Word
FREE 14+ Sample Sales Call Reports in PDF Apple Pages ...
FREE 10+ Hospital Incident Report Samples [ Serious, Nursing ...
FREE 6+ Staffing Model Samples in PDF Excel
FREE 4+ Nursing Business Plan Samples [ School, Service, Agency ]
FREE 8+ Nursing Assessment Samples in PDF PPT
FREE 10+ Hospital Discharge Summary Samples [ Patient, Therapy ...
FREE 12+ Job Profile Samples & Templates in MS Word PDF